
This is an extended version of our interview with Boulder Cardiologist Nelson Trujillo. For the broadcast version, go here.
Producer: Shelley Schlender
Podcast: Play in new window | Download (Duration: 56:21 — 77.4MB)
Subscribe: RSS
The KGNU Science Show

This is an extended version of our interview with Boulder Cardiologist Nelson Trujillo. For the broadcast version, go here.
Producer: Shelley Schlender
Podcast: Play in new window | Download (Duration: 56:21 — 77.4MB)
Subscribe: RSS
This is Shelley Schlender’s extended interview of Larry Gold, founder of the GoldLab Symposium. For the broadcast version, go here.
Producer: Shelley Schlender
Podcast: Play in new window | Download (Duration: 44:56 — 61.7MB)
Subscribe: RSS
DE-FUNDING SCIENCE
National Institute of Standards
Atomic Spectroscopy Group
TRANSCRIPT of KGNU Science Show April 22, 2025
Shelley Schlender [00:00:13] I’m Shelley Schlender. This is How on Earth, the KGNU Science Show. Today is Tuesday, April 22nd, 2025. Coming up, we look at federal cutbacks of a group that provides the entire world with accuracy measurements that help with everything from better smartphones to finding exoplanets. It’s the defunding of the National Institute of Standards and Technologies Atomic Spectroscopy
Alexander Kramida – Atomic Spectroscopy Group [00:00:41] We receive hundreds of letters suggesting support. Most of them are from abroad. China, of course, they are very generous in their suggested salaries and so on, but we don’t want to move to China.
Shelley Schlender [00:01:01] I’m Shelley Schlinder. This is a year with many cutbacks in federal funding. Time is running out on funding for many scientists. As part of that, we’re going to look today at one small band of accuracy experts who create crucial standards for scientists around the world. These experts are with the National Institute of Standards and Technology, also known as NIST. NIST has offices here in Boulder that are getting federal cutbacks right now. And also offices in Maryland that are getting cutbacks. So what is NIST? To understand its overall mission, check the clock on your smartphone, on your computer. They’ll show the same time, thanks to NIST’s incredibly accurate atomic clocks. The National Institute of Standards and Technology also maintains accuracy on complex things like GPS coordinates. You know, what you use for mapping and something that most people don’t know anything about, something called atomic spectroscopy. To understand a spectrum, picture a rainbow. That beautiful arc of colors, happens when water droplets refract sunlight into its visual spectrum. Every rainbow has the same colors. It’s the fingerprint of sunlight refracted through water. When it comes to atoms, spectra get more invisible and complicated. Atomic spectra involve the patterns of light energy that come out of or go into an atom. Each atom has a unique spectrum. Each ion of that atom has its own unique spectrum and so on. These unique fingerprints provide crucial IDs and calibration for etching, advanced macrochips for detecting a missile launch, for finding exoplanets. Through the National Bureau of Standards and Technology, the Atomic Spectroscopy Group has maintained a database about this information that’s free to anyone around the world. The Atomic Spectroscopy Group database is so important it’s one of the top three most frequently accessed datasets at NIST. Last month, the federal government sent out notices that it is shutting down this atomic spectroscopy group. Here’s an overview of what’s happening from How on Earth volunteer Joel Parker.
Joel Parker [00:03:29] I’m Joel Parker with How on Earth. In my research work as an astronomer, I have been on many projects that used the database from the Atomic Spectroscopy Group, including studies of the chemical compositions of comets and planets. It appears the reason given for closing the group was that their work is not considered to be statutorily essential for the National Institute of Standards mission. The mission stated on the NIST website seems to be exactly the kind of services that the Atomic Spectroscopy Group provides. According to their website, the National Institute of Standards and Technology, or NIST, is one of the nation’s oldest physical science laboratories, founded in 1901, and is now of the U.S. Department of Commerce. Congress established the agency to remove a major challenge to U.S. Industrial competitiveness at the time, a second-rate measurement infrastructure that lagged behind the capabilities of the United Kingdom, Germany, and other economic rivals. The NIST mission statement is to promote U. S. Innovation and industrial competitivness by advancing measurement science standards and technology in ways that enhance economic security and improve our quality of life. The work performed by the Atomic Spectroscopy Group fundamentally is measurement science and standards. For How on Earth, I’m Joel Parker.
Shelley Schlender [00:05:13] Thanks to Joel for that summary. To catch up on what’s happening, last Friday I talked with a member of the Atomic Spectroscopy Group in NIST’s Maryland offices.
Alexander Kramida – Atomic Spectroscopy Group [00:05:25] Alexander Kramida. That’s how I pronounce it in English. I am originally from Soviet Union, born in Ukraine.
Shelley Schlender [00:05:34] Alexander Kramida is a lean man with graying hair. On our Zoom call, he sat in a windowless office surrounded by file cabinets and research papers. It was a small office. He looked determined but weary. Here is Alexander Kramida.
Alexander Kramida – Atomic Spectroscopy Group [00:05:50] That’s how we know about the stars. We are looking at the light, they emit or absorb and we are deciphering their composition and their history and can make projections what will happen with the star.
Shelley Schlender [00:06:05] Now I understand all of these things best when I think about arcs of color, but the spectrums that you understand have a lot more data in them, mathematical calculations throughout it that can tell all kinds of things about what that spectrum is.
Alexander Kramida – Atomic Spectroscopy Group [00:06:21] Since you mentioned calculations, I would need to, how to say, disappoint you a little bit, because practically nothing about the spectra can be calculated. Almost all the knowledge comes through experimental analysis.
Shelley Schlender [00:06:36] Look at how much you know about this and I don’t. You’re saying you constantly have to compare experiments so that everybody can come to a single place in the world and see what is the spectrum because so many things have some spectrums associated with them.
Alexander Kramida – Atomic Spectroscopy Group [00:06:53] Yes, whenever you have something hot, it emits light. The hot plasmas, which are ionized gasses are used in so many different things, like plasma torches, for example, for welding, or if you need to process the semiconductor chips, you use some plasmos for etching.
Shelley Schlender [00:07:21] Oh, that’s right, when somebody uses a smartphone, when somebody is planning to make a special missile for, those have microchips in them. A car that has windshield wipers has a microchip in it, and that has one of those microchops that has been etched using one of these plasma machines that you can test to see if it’s working right with the spectrum that it produces.
Alexander Kramida – Atomic Spectroscopy Group [00:07:48] Yes, you get it. You said you have no scientific background, but you are grasping it.
Shelley Schlender [00:07:54] For fusion reactors, for instance. There’s a great deal that needs to be done to figure out the spectrums where those work at the best potentially.
Alexander Kramida – Atomic Spectroscopy Group [00:08:03] This is one of the most important applications. Developing fusion can save the Earth from ourselves, from our waste overheating the Earth. We need to reduce those wastes. Thermonuclear fusion is a very good way to do that.
Shelley Schlender [00:08:23] Your database that 70,000 scientists around the world access every month, your database and you scientists to maintain it, is in danger of being shut down.
Alexander Kramida – Atomic Spectroscopy Group [00:08:36] Not completely shut down. This database will continue to stay on in its frozen state. My belief is that it’s not realistic because everything breaks when you get a new software update on your computer, something stops working and there will be nobody to repair it.
Shelley Schlender [00:08:55] 70,000 scientists a month look and refer to this database. And you’ve just told me that because of the federal cutbacks and the fact that the staff at your center are to be laid off, the database will continue in a frozen state, meaning that people can look at it, but it won’t have any updates or repairs.
Alexander Kramida – Atomic Spectroscopy Group [00:09:18] Yes, that’s exactly right. And this current state is, in my opinion, very meager. To give you some understanding, atomic spectra cover not only neutral atoms, but also ionized. Not only singly ionized, but multiply ionized as well. So if you count how many spectra there are in principle, you have about 100 chemical elements in the periodic table. And you would think that highly charged ions, say 50 times ionized uranium or something like that, are some exotic thing. But no, they are becoming the focus of new developments related to high precision measurements and fundamental.
Shelley Schlender [00:10:05] Okay, what you’re telling me I think is that person who’s just thinking, let’s cut back the money and the cost, would say, well, this database, we already know what all the elements are. This database already has all the information. Why would we need to update it? And what you are saying is that science is constantly discovering nuances of each atom. For instance, these ions, and scientists around the world and technologists are new technologies that depend. On knowing precisely what each change in these ions might do. And that’s the current state of the art. And who knows what next year will bring. People really need access to shared data about new spectrums. Is that close?
Alexander Kramida – Atomic Spectroscopy Group [00:10:52] Yes, you are right in some aspects, but that’s not all of it. In our database, in the present state, we have some information, only about 20%, maybe even less, of all possible spectra. The rest is completely unknown, and people are working on that and publishing papers with a steady stream of about 500 papers a year. And just to analyze this information, it needs dedicated work, very difficult work. We are doing that. What is currently happening is that we are ordered to stop this.
Shelley Schlender [00:11:33] You are ordered to stop that at the National Institute of Standards and Technology.
Alexander Kramida – Atomic Spectroscopy Group [00:11:38] Yes, that’s right.
Shelley Schlender [00:11:40] Dr. Kramida, if your database is not kept constantly up to date, it means that for scientists around the world, sure they can find it in scientific papers themselves, but they don’t have a shared consensus. So instead of going, oh, that’s where the latest information is, they’d have to spend hours each one of these 70,000 scientists a month going and trying to analyze this themselves. It would slow down advancements in science and technology a great deal. Not to have you all working on what you’re working on.
Alexander Kramida – Atomic Spectroscopy Group [00:12:12] That’s partially right, but you said looking for the latest. The latest is not always the best. The best is something that has the greatest precision, the greatest accuracy. People who are applying this data do not necessarily have the expertise to decide what is the best, we have this expertise. Our database is the only one in the world providing critically evaluated data for atomic spectra.
Shelley Schlender [00:12:41] Meaning that it’s data that people can trust, and is this free to all scientists around the world?
Alexander Kramida – Atomic Spectroscopy Group [00:12:46] Exactly, that’s why all scientists everywhere in all kinds of applied fields, they trust our database. We have the expertise and knowledge needed to recommend the data.
Shelley Schlender [00:12:59] How many scientists and technicians are part of the atomic spectroscopy group that you’re the manager of?
Alexander Kramida – Atomic Spectroscopy Group [00:13:05] Our group is currently tiny, it’s just six people.
Shelley Schlender [00:13:09] Just six people. Have you been asking for more people?
Alexander Kramida – Atomic Spectroscopy Group [00:13:13] Of course, but this goes on for decades already. Our funding is frozen at the level of, say, 1970. But the salaries are growing due to inflation. And so we have less and less people that we can support.
Shelley Schlender [00:13:30] Your staff has already been dwindling. I hear that you all have to buy your own coffee for the break room.
Alexander Kramida – Atomic Spectroscopy Group [00:13:36] Yes, this is an ancient tradition.
Shelley Schlender [00:13:39] I’m looking at your office there in Maryland. It doesn’t look like a fancy office. It looks like a lot of file cabinets. It’s not the penthouse suite.
Alexander Kramida – Atomic Spectroscopy Group [00:13:48] We are dedicated to what we are doing and comfort is not available for us.
Shelley Schlender [00:13:54] There has been a Nobel Prize winning scientist who said it would be idiocy to shut down your group. Has this made any difference?
Alexander Kramida – Atomic Spectroscopy Group [00:14:04] We have already resigned. There is no change in plans. The laboratory and NIST directors, they have orders from above and they have to follow the order.
Shelley Schlender [00:14:15] You have already resigned.
Alexander Kramida – Atomic Spectroscopy Group [00:14:16] Yes, the deadline for submitting applications for retirement was yesterday. It was an act of grace, I would say, to allow us to retire to our notices. That’s what people are getting in other agencies. We are in a better position somewhere.
Shelley Schlender [00:14:35] We’re speaking on Friday. That means that Thursday is the day that you resigned.
Alexander Kramida – Atomic Spectroscopy Group [00:14:42] Yeah, a few days before that.
Shelley Schlender [00:14:45] Oh my goodness, does this mean that you were given an option that gave you a chance to have a retirement fund? You still get paid.
Alexander Kramida – Atomic Spectroscopy Group [00:14:55] It’s not much.
Shelley Schlender [00:14:58] It’s not much, um, hmm, it’s already done.
Alexander Kramida – Atomic Spectroscopy Group [00:15:02] It’s already done.
Shelley Schlender [00:15:04] You are there at your office. Did your email shut off? I’ve heard of that happening at some agencies where email shuts off, you get locked out of your office, but you’re there.
Alexander Kramida – Atomic Spectroscopy Group [00:15:15] My day of retirement is April 30th, so until that day, I’m in the office trying to save as much as I can because we have vast archives, hundreds of years of research. Hundreds of years research. Coping it and saving it with the intent to continue what we are doing from home or from other places.
Shelley Schlender [00:15:39] I’m Shelley Schlender. This is How on Earth, the KGNU Science Show. Today we’re getting a window into cutbacks in federal science funding by talking with Alexander Kramida. He’s a member of the National Institute of Standards and Technologies Atomic Spectroscopy Group. It sets measurement standards critical for everything from microchip manufacture to ways to detect the launch of an atomic missile. When news came out last month that the federal government is shutting down this group Change.org created a petition of protest. It includes these words from Nobel Prize winner Sheldon Glashow.
Sheldon Glashow (from Change.Org website) [00:16:16] I won the Nobel Prize in Physics some 50 years ago, and NIST has always played a fundamental role in basic science. I don’t think that the progress in science would have been as great without it. I cannot imagine that our government could be stupid enough to castrate this gem.
Shelley Schlender [00:16:42] As of last week, Change.org’s petition to save the Atomic Spectroscopy Group had over 5,000 signatures of support. One letter of support had ended with the words, “With enough voices from the worldwide scientific community, we should be able to prevent this catastrophe.” The spectroscopy group is still being shut down by the federal government. Here’s more from the manager of the Atomics Spectroscopic Group, Alexander Kramida.
Alexander Kramida – Atomic Spectroscopy Group [00:17:11] We won’t get paid, maybe, or maybe we will. We don’t know yet.
Shelley Schlender [00:17:16] Right now, for free, you’re helping hold this information together about what the spectrums are because we need that for making better microchips, for better welding devices, for better pretty much anything that has high tech to it.
Alexander Kramida – Atomic Spectroscopy Group [00:17:31] Yes, that’s right.
Shelley Schlender [00:17:34] Oh, this is not an easy conversation to have, meaning that it’s not easy to talk about something that is closing down.
Alexander Kramida – Atomic Spectroscopy Group [00:17:41] Well, it’s closing down in this place, but it will surely continue in other places.
Shelley Schlender [00:17:47] Will it continue with the group that you have?
Alexander Kramida – Atomic Spectroscopy Group [00:17:50] We need more.
Shelley Schlender [00:17:51] You need some new young scientists.
Alexander Kramida – Atomic Spectroscopy Group [00:17:53] It’s a little bit difficult to involve young scientists in light of what’s happening with us.
Shelley Schlender [00:17:59] Tell me why young scientists don’t want to join you in your group.
Alexander Kramida – Atomic Spectroscopy Group [00:18:03] Because it’s being shut down.
Shelley Schlender [00:18:05] Yes. Well, there is that. But if universities say, this is crazy, we can’t do without this. Or if industry were to say, we’re going to fund this ourselves.
Alexander Kramida – Atomic Spectroscopy Group [00:18:18] Yeah, that would be wonderful. You know, as government employees, we cannot engage in any job search or whatever when we are working. So it’s all in the future. Maybe when we will be free of the government rules, we will start.
Shelley Schlender [00:18:35] My guess is that a lot of this information about spectroscopy, there would be a competitive advantage to one big company having a database and keeping it from other people. Maybe they would share their information or maybe they would not.
Alexander Kramida – Atomic Spectroscopy Group [00:18:48] If it is in our power, we will do all we can to prevent this, because everything we are doing is open, open for everybody. And that was the good feature of the government position, because all the data produced by U.S. Government are free for everybody’s use by law.
Shelley Schlender [00:19:08] People will still be able to see the frozen database, the one that the government is holding still, like a piece of fossilized trees or something. You know, it’s being held still at this moment in time. What are you going to do if you find funding where you have to say, this database is the one that’s now being updated?
Alexander Kramida – Atomic Spectroscopy Group [00:19:27] Yes, that’s the first thing we are going to do. We are going arrange a mirror site which will continue to be developed. Yes, we need the new young minds to train them and eventually replace us. There are so few of us and the expertise is not something attained easily.
Shelley Schlender [00:19:46] How many years have you been doing this, Dr. Kramida?
Alexander Kramida – Atomic Spectroscopy Group [00:19:49] 50 years.
Shelley Schlender [00:19:50] You’d like to see some new people coming in and doing this. Well, if this was in my neighborhood, I would put a GoFundMe site together and say, who wants to help fund my project? But I’ve got a feeling that… Atomic spectroscopy lab would take more than what people usually get on a GoFundMe site.
Alexander Kramida – Atomic Spectroscopy Group [00:20:15] We’ll see what happens. We have a dedicated person who is trying to do all these political arrangements. This is Dr. Yuri Rolchenko. He is responsible for all this. I cannot say anything about what will happen. It’s all too nebulous at the moment.
Shelley Schlender [00:20:34] It’s nebulous and it’s perhaps a little bit secret right now that people don’t want to show their hand yet on how they might help out.
Alexander Kramida – Atomic Spectroscopy Group [00:20:42] We receive hundreds of letters suggesting support. Most of them are from abroad. The German agency equivalent to NIST, which is the National Bureau of Standards, they are offering us positions. China, of course, they are very generous in their suggested salaries and so on, but we don’t want to move to China.
Shelley Schlender [00:21:06] So you’re getting enthusiastic letters of, we’ll help you out. Come join us from Germany and from China.
Alexander Kramida – Atomic Spectroscopy Group [00:21:14] From different places.
Shelley Schlender [00:21:15] And are these places saying, we will help you set up something where you can share the database with the world or are some of these places saying come to us, we’ll keep some of this secret.
Alexander Kramida – Atomic Spectroscopy Group [00:21:26] Nothing of the sort all suggestions that we have have this provision that the data will be open for everybody
Shelley Schlender [00:21:34] Countries like China and Germany are saying, this is a valuable resource. We want to support it. Come live with us, come live in our country where we believe this is so important. We will fund this, since the United States is saying they will not.
Alexander Kramida – Atomic Spectroscopy Group [00:21:48] Yes, but there is a legal problem with that, because all the data that we have in the database technically belongs to the Department of Commerce. They have the copyright and they have the right to decide if they allow it to be moved somewhere else or not, and they are not allowing to move it abroad.
Shelley Schlender [00:22:08] So there’s a catch-22 for taking the offers of these other countries. You know, we hear about this that if science is not funded in the United States, that many of the greatest minds in the U.S. Will be drawn to other countries, that’s really happening.
Alexander Kramida – Atomic Spectroscopy Group [00:22:26] Yes, indeed. So we are sure that we will be okay personally, it’s okay. It’s not our personal fate that bothers us. The fate of the fundamental science is the most important thing.
Shelley Schlender [00:22:41] Do you think there’s any possibility of going back to the federal government and whoever it is who sent you those resignment letters? And they would say, we’ve changed our mind. We would like you all to keep working right where you are again.
Alexander Kramida – Atomic Spectroscopy Group [00:22:55] Apprehensive of this prospect. Right now, it is not a good place for us. It’s not the first time that we were given this attitude of treating our field as not being important. And that’s despite the fact that our database is the third one at least, the number of queries.
Shelley Schlender [00:23:18] Your database about atomic spectroscopy is the third most commonly accessed one at NIST.
Alexander Kramida – Atomic Spectroscopy Group [00:23:23] Despite that, a few years ago when Congress proposed to cut the National Institute of Standards and Technology, the NIST Directorate issued a memorandum suggesting that several fields will be cut off, and the first one of them was our atomic spectroscopy group. It’s not a news thing, it’s the first time these threats came through.
Shelley Schlender [00:23:49] Who was the president when the first threat came through?
Alexander Kramida – Atomic Spectroscopy Group [00:23:52] I will not speak about presidents because as a government worker, I am not allowed.
Shelley Schlender [00:23:57] What year was the first threat?
Alexander Kramida – Atomic Spectroscopy Group [00:23:59] About five years ago now, I don’t remember exactly.
Shelley Schlender [00:24:03] Not that you have to say, but I would say five years ago, the president was a guy named Donald Trump.
Alexander Kramida – Atomic Spectroscopy Group [00:24:09] It’s not my field to talk about politics.
Shelley Schlender [00:24:13] Yeah, I understand. Well, so you have heard threats about being shut down before, and it’s hard to keep working with the uncertainty that maybe some group would change their mind and then say, please come back, and then you don’t know how soon it will be before they say, no, you’re gone. You need more certainty than that. And by the end of this month, this office that I’m seeing you in with all these papers, that basically will be gone. Yes. I’m hopeful that your determination to keep this database fresh and continuing means that within a few months, there will be a new database that’s a mirror of the old one that has more information that’s new in it, because you’ve gotten funding in a place to be here in the United States. My best to you. And please, if you have some news, send me an email and we’ll share it on the air.
Alexander Kramida – Atomic Spectroscopy Group [00:25:22] I’ll do that.
Shelley Schlender [00:25:27] I’m Shelley Schlender. We’ve been speaking with Alexander Kramida. He’s manager of the Atomic Spectroscopy Group, part of the National Institutes of Standard and Technology. At the end of this month, the federal government is closing down the group and freezing their database. Kramida says that they’re looking for a way to keep the database going and update it that does not depend on funding from the federal governments.
Shelley Schlender [00:26:12] That’s all for this edition of How on Earth. Our executive producer is Joel Parker. This week’s show was produced by me, Shelley Schlender. Additional contributions from Joel. Our theme music was written and produced by Josh Cutler. Additional music from John Adams. Visit our website at howonearthradio.org to find past episodes, extended interviews, and you can subscribe to our podcast through iTunes and follow us on Facebook, Blue Sky NX. Questions or comments? Want to get involved? Send us a note through our website for How on Earth, the KGNU Science Show. I’m Shelley Schlender.
This is an extended interview with CU Boulder Wildlife Expert Marc Bekoff about challenges and possibilities with Colorado Wolf Reintroduction. For the broadcast interview, GO Here. And here is an AI-generated written transcipt.
Podcast: Play in new window | Download (Duration: 51:38 — 70.9MB)
Subscribe: RSS
This is an extended version of the interview with Rick Johnson, author of Nature Wants Us to Be Fat.
TRANSCRIPT BELOW:
RICK JOHNSON [00:00:00] My name is Richard Johnson. I’m a professor of medicine here at the University of Colorado.
SHELLEY [00:00:04] In fact, you direct the Department of Hypertension, or have you changed your position now?
RICK JOHNSON [00:00:09] I was the chief here from 2008 till 2017, but currently I’m simply a professor.
SHELLEY [00:00:17] That gives you more time to research and less that you have to be directing.
RICK JOHNSON [00:00:20] Absolutely correct.
SHELLEY [00:00:22] Are you doing a lot of research?
RICK JOHNSON [00:00:23] I am. I continue to be a researchaholic. I’ve been doing research since the early eighties. It makes up a great part of my life. It’s exciting, exhilarating and hard work.
SHELLEY [00:00:38] It is all those things with a lot of mysteries, a lot of dead ends, a lot of sudden doors that open up.
RICK JOHNSON [00:00:44] It’s been a series of great surprises and discoveries. The best I can say is that this whole story that I’ve written about is like finding treasure, I found a piece of gold. And we thought that was the best thing in the world. And then we found another one, and then we found another. And then we found a whole treasure chest. It’s sort of like finding King Priam’s treasure. What we’ve realized is that this pathway that we’ve identified seems to be involved, not just in obesity and diabetes, but in many, many current diseases, having a role in cancer and having a role in dementia and other medical problems.
SHELLEY [00:01:22] Backing up just a little bit. You’re in the Division of Hypertension and Nephrology, which means that you deal with things like high blood pressure and kidney disease and gout.
RICK JOHNSON [00:01:36] Yes, that’s right. So I started primarily in the world of kidney disease and high blood pressure. But as my research progressed, I migrated into other fields and ended up studying metabolic syndrome, obesity, diabetes and other conditions.
SHELLEY [00:01:55] Metabolic syndrome is that very strange thing where somebody’s metabolism gets out of balance and they get really hungry for things that they don’t really need. They lose energy. They can’t build muscle as much. They’re more prone to heart disease.
RICK JOHNSON [00:02:10] Yeah, metabolic syndrome refers to a constellation of findings and usually it includes abdominal obesity, high blood pressure, elevated blood sugar, sort of like insulin resistance. So it’s not true diabetes, but it’s sort of pre-diabetes.
SHELLEY [00:02:29] Cells their body can’t take in energy, and the insulin levels are very high.
RICK JOHNSON [00:02:37] You become resistant to the effects of insulin. So the insulin levels go up to help control your blood sugar. But even with that, your blood sugars tend to be a little bit on the high side and then you have elevated triglycerides in your blood, which is fat, and oftentimes you’ll have fatty liver. And this constellation of signs got the name metabolic syndrome many years ago. We now know that about a quarter of all adults have metabolic syndrome in the U.S. and some places in the world. It’s higher. So it seems to be a real common issue.
SHELLEY [00:03:12] In the US it’s common, but in some parts of the world. It’s lower, though.
RICK JOHNSON [00:03:15] Absolutely. So it can be lower. It’s sort of like, in our country, diabetes is present in about 10 to 12% of the population. You go to Samoa, it’s like 40%. You go to Kuwait, it’s like 25%. You study the Pima Indians where it’s 50%. And so diabetes and metabolic syndrome, which kind of run together. they vary quite a bit. We have very high rates here compared to some places like Sweden, but it’s still low compared to countries like Kuwait, Samoa and so forth.
SHELLEY [00:03:52] It isn’t good, but it could be worse.
RICK JOHNSON [00:03:54] It could be worse.
SHELLEY [00:03:55] Rick Johnson, you’ve written some other books. One, you’ve called The Fat Switch. One, you called The Sugar Fix. And now you have a new book called Nature Wants Us to Be Fat.
RICK JOHNSON [00:04:10] Yeah. So this book is the culmination of the work I’ve been doing for the last 20 or 30 years. It’s told like a detective story because that’s sort of the way it was when we tried to figure this out. And it takes us on an adventure story where we try to figure out what causes obesity. We begin by including studies of animals in nature that naturally become obese. We try to figure out why they become obese, and then we relate it to humans. And from that, there were many discoveries. Some of them are very surprising about what causes obesity. And from that comes a whole series of ways to treat obesity, many of which have not been tried before. And we have some data that some of these methods will work. And we’ve also been able to link this pathway of metabolic syndrome, not just with, you know, classic things like diabetes, obesity, high blood pressure and heart disease, but also, as I mentioned, with things like behavioral disorders, with dementia, with alcoholism and with cancer.
SHELLEY [00:05:17] So many paths lead to similar roads sometimes.
RICK JOHNSON [00:05:21] Yeah, it’s sort of like we identified a major, major mechanism that animals use to become fat. And this mechanism is involved in a lot of diseases. And so I think it will turn out to be important in terms of how we approach a lot of our current diseases.
SHELLEY [00:05:43] Let’s start with the punch line. What do you think animals do to get fat?
RICK JOHNSON [00:05:49] They can do a variety of things, but our first big breakthrough was the discovery of the importance of fructose. Fructose is known as fruit sugar; in the wild it’s and fruit and honey. Perhaps many of you are going, ‘Hey, wait a minute, because aren’t fruits supposed to be healthy? I thought honey was healthy.’ It will sound sort of funny to hear that fructose might actually be at the core of what’s driving the whole, you know, metabolic syndrome and related diseases. But it turns out that it really is fructose. And we’ve been able to show how and we’ve also been able to show why natural fruit intake for us is actually healthy. And yet when animals eat a lot of fruit, they become fat.
SHELLEY [00:06:43] There’s a lot to unpack in all of that. Let’s start with the concept, animals want to be fat. Given how much Americans try not to be fat, why do animals want to be fat?
RICK JOHNSON [00:06:57] The title’s not completely true. Only some animals want to gain fat, and that’s to protect them during periods of food shortage. Most animals will actually try to maintain a small amount of fat, and they’ll regulate it very well. So they’ll have some fat, but they don’t want to get truly obese. And so what most animals do, if they eat too much one day, they’ll eat less the next. If they exercise and run around too much one day and burn too many calories, the next day, they’ll slow down and balance out . . . other than what they expected to do. You know, if they’re actively growing, you can show that by taking an animal and force feeding it so that it gains weight or you can fast an animal so it loses weight against its will. And then if you stop that, they go right back to the weight they should be at that time of the year. So not even goes back to the way they were. They’ll go back to the weight where they feel they should be for that time of the year. But there are animals that want to gain weight, and they do it at specific times. The classic is the animal preparing for hibernation.
SHELLEY [00:08:09] Oh, yes. Those bears that get so big before they go to sleep.
RICK JOHNSON [00:08:13] Yes. So a bear, for example, will maintain its weight during the summer, but in the fall, suddenly it will become hungry. Really hungry. It can gain as much as eight or ten pounds a day. They can be eating 20,000 calories a day and they will increase their weight as much as 50%. And the way they tend to do it is by eating a lot of fruit. We think of fruit as healthy, but we are eating. You know, how many berries or grapes do you eat, Shelley?
SHELLEY [00:08:48] I don’t eat very many grapes, actually.
RICK JOHNSON [00:08:50] Let’s say you eat a bowl of grapes. You know, bears getting ready to hibernate will eat 10,000 grapes in 24 hours. So we’re talking a different level of fruit. Orangutans, when they want to gain weight, they’ll eat fruit and they’ll gorge. And I mean, they’ll get into a tree and they’ll eat fruit after fruit after fruit and eat it fast and consume and get a lot of sugar. Normally, a fruit will have like five grams of fructose, maybe ten. When we’re eating fruit, we tend to eat only, you know, one or two fruit at a time. But a bear or a orangutan or an animal that wants to eat fruit to gain weight, they’ll eat a lot more relative to their weight. They’re getting a lot more sugar. I’m calling that sugar, but it’s fruit sugar, also known as fructose. That’s what makes fruit sweet. And animals that want to gain weight will pick ripe fruit, and ripe fruit has more sugar. When a fruit ripens, the sugar content goes up. And when that happens, the fructose will increase. Also good vitamins tend to go down as the fruit ripens. So things like vitamin C tend to decrease as a fruit ripens. Vitamin C actually can block some of the effects of fructose. In the early part of when the fruit is just beginning to grow, it’s very tart. It has a lot of fiber, potassium, all these things that slow the absorption of fructose. so it discourages animals to eat it because they’re not going to get that much sugar. But as the fruit ripens, the sugar content goes up, the vitamin C content goes down, the all the other good things go down. And now the fruit is more suited to stimulate this metabolic switch where they start gaining weight and become hungry and so forth. That’s sort of how it works. So the animals that eat a lot of this fructose trigger a biologic switch. And this was what we been trying to uncover, an actual biologic mechanism that triggers weight gain, obesity, insulin resistance, a rise in blood pressure, all the features of metabolic syndrome, and they’re all all there to help us survive. When I was taught about metabolic syndrome, when I was a medical resident, it was told to me as something that’s pathologic. You know, insulin resistance is not a normal thing. We shouldn’t be insulin resistant. Metabolic syndrome is a disease. Actually, it’s not a disease. It is a normal biologic process that animals trigger when they need to gain weight.
SHELLEY [00:11:54] That was so interesting to read in your book. Nature Wants Us To Be Fat, about the animals that migrate, such as geese. When they prepare for migration, they get fatty livers. If people get stuck with these conditions, they’re really sick. But the geese only have the fatty liver when they’re traveling lots of miles and they need the extra energy. Humming birds! Every day, they end up at the end of the day with a fatty liver, but then they burn it up overnight and go back to needing more food. And so they’re very robust in being able to handle things that would cause metabolic syndrome, in us. Meanwhile, hummingbirds, their blood sugar goes up above 400.
RICK JOHNSON [00:12:36] They basically become diabetic and fat during the day when they’re drinking sugar water and then they burn it off at night despite the fact that they are so metabolically fit. If they drink pure sugar water all day long, their livers turn pearly white, ‘the fattest of all livers of birds’, one researcher wrote, and they develop frank diabetes and then they burn it off. It’s an amazing story about the power of sugar, that it can take an animal that is so metabolically fit and cause them to become diabetic–hummingbird feeders. So you put sugar water to get the sugar. Water and nectar are pretty much the same.
SHELLEY [00:13:16] A hummingbird can basically become a diabetic by the end of the day, but by the next morning they’re so healthy and burned it all off. The fats and all of the metabolic symptoms of what we call diabetes, that they just start fresh the next day.
RICK JOHNSON [00:13:33] Exactly. And here’s a really interesting story, Shelley. Fruit flies are flies that love fruit and they eat fruit and that’s pretty much fruit juice. But there’s other things in the fruit. If you switch a fruit fly to pure sugar, it will become obese. They’ve actually shown that flies will become diabetic and obese.
SHELLEY [00:13:58] A fly can become obese and diabetic?
RICK JOHNSON [00:14:01] Yeah. And then they die.
SHELLEY [00:14:04] As you think about it, a fly is trapped inside of an exoskeleton. So it would cause all kinds of extra pressure and problems for it to become obese.
RICK JOHNSON [00:14:14] Yes, it’s true. Ants will become fat if they eat sugar. You can’t tell because they’ve got this exoskeleton. So the fat’s inside. But ants can become quite fat from sugar. And there are some ants that will search out sugar. They love sugar more so than other types of foods.
SHELLEY [00:14:35] Rick Johnson I hear you saying that natural sugars found in the wild as fruit and berries generally are okay for animals, but our human style of sugars, even some of the animals that are used to sugars, it’s too much for them.
RICK JOHNSON [00:14:48] So refined sugar probably can overwhelm animals and nature.
SHELLEY [00:14:53] Does it overwhelm us as humans?
RICK JOHNSON [00:14:55] Absolutely. For sure it does.
SHELLEY [00:14:57] But Rick Johnson, refined sugar is in most of our foods.
RICK JOHNSON [00:15:01] Yes, it is. And most of our foods In fact, 70% or more of processed foods have sugars put in them. And you want to know something really interesting/ If you take an animal and you knock out its sweet taste so it can’t taste sweet, it will no longer care for artificial sugars like Splenda. Sugars wont give it any kind of dopamine surge. There’s no pleasure with that. But those animals with the sweet sensation knocked out still will seek out sugar water even though they can’t taste it. We found that it’s because when you drink fructose, for example, the metabolism of fructose is what’s involved in the craving response for fructose.
SHELLEY [00:15:44] It’s not our taste buds? Rick Johnson,so many people say that we have been doomed as a human population because we have enough food, and the food just tastes so delicious. So of course, people eat too much. You’re saying something different?
RICK JOHNSON [00:16:06] It’s a little bit more complicated than that. So we have five tastes. One is sweet, one is salty, one is savory–umami, and there’s bitter and sour. So there’s actually three tastes that we really like sweet, salty and savory. And the other two are sort of meant to help us avoid foods that are bitter or sour because many times they’re not good for us. Now the sweet is your sugar, right? What we know is that if you knock out the sweet receptor, animals will still like sweet food. And that’s because of the metabolism. They will reduce how much sugar they eat, they’ll eat less sugar. But if you give them a choice between sugar water and regular water, they will be able identify the sugar water even though they can’t taste that it’s sweet.
SHELLEY [00:16:59] Rick Johnson, other scientists who’ve studied sensing molecules inside of our bodies report that sensing receptors on cells in our digestive tract, are very similar in their makeup to the taste bud receptors on our tongue. So when you knocked out that taste of sugar in lab animals, is that just referring to taste receptors for sweet on tongue or is that referring to all of these receptors for that kind of substance?
RICK JOHNSON [00:17:29] So it turns out that the study that was done where they knocked out the sweet receptors included the taste bud sweet receptors, but there are sweet receptors in the gut. However, we here at CU Denver knocked out just the taste, only the taste, leaving the sweet receptors intact in the gut. And we knocked out all taste. And when we did that, the animals still like sugar.
SHELLEY [00:17:57] You did this with mice?
RICK JOHNSON [00:18:00] Yes. And what we found is that if you knock out the taste receptor, you reduce the amount of sugar you eat, but you still become obese from sugar. And sadly, you become more sensitive to the effects of sugar. So you eat less sugar, but you’ll still become more obese.
SHELLEY [00:18:16] That’s another part of your story that we’ll get to in just a moment. I want to keep giving people the punch line, though, which is that your research has shown that if people reduce their consumption of sugary drinks, plus foods that have added sugar, it can do a huge benefit for their health. But if someon’e health is already broken somewhat by these kinds of foods, there may be other things they need to pull out of their diet as well. That’s a quick summary. Is that fair to say?
RICK JOHNSON [00:18:47] Not fully. Fructose sugar is the PRIMARY driver of obesity. You’re totally right in that part. Sugar or high fructose corn sirup make up about 15% of our diet. Some children are eating 25% of their food is sugar. Children, adolescence and also disadvantaged populations are often eating a higher percentage of sugar. And so fructose-based sugar is your number one driver. You’re right. But there are other drivers of obesity, and they’re very important. So I don’t want to say that they’re distant second or third. They are involved. Originally, when we were studying this, we were thinking, hey, it’s all sugar, you know? And so my first book (The Sugar Fix), hey, let’s just cut out sugar and fructose. But it wasn’t enough. It’s not enough.
And that is because of the sad discovery by our group that there are other foods that trigger this switch, the survival switch. And this switch can be triggered by foods such as high glycemic carbs, bread. Rice, potatoes and chips. These foods do not contain fructose, but they actually can trigger the switch. And what we found is that the way they work is they stimulate the production of fructose in the body. So it isn’t just about the fructose we eat. It’s about the fructose we make. And no one was really thinking of foods as working by causing us to make fructose. Everyone was thinking it was the foods we were eating.They were thinking it’s the carbs and the protein and the fat. But it turns out that these carbs, which we call high glycemic carbs, when you eat them, they release glucose and the glucose gets into the blood and your normal glucose (in your blood) is like 80 to 100. But when you eat a high glycemic carb, the glucose in the blood can go up transiently, maybe to 120, 140 or 150, but it’s transient. So everyone just says, well, don’t worry about it. Or if you do worry about it, they say, Well, the problem is that it stimulates insulin and insulin puts fat on you. And so the thought is that high glycemic carbs could be a cause of obesity, primarily through this mechanism (of raising insulin). But what we found is that when the when the glucose levels go up, that triggers the body to make fructose from the glucose. And the glucose can be converted to fructose through a chemical reaction. And we call that reaction the polyol pathway.
SHELLEY [00:21:49] Polypll sounds like everything thrown in, including the kitchen sink, poly all that.
RICK JOHNSON [00:21:54] So it sounds like that; it was a name given to it a long time ago, but it’s been known that the body can make fructose, but no one thought it was important. What we found is that that a number of foods trigger the production of fructose in the body and animals use this so not all animals eat fruit to become fat. There are animals that don’t eat fruit that become fat other ways. One way is high glycemic carbs. They will cause obesity.
SHELLEY [00:22:22] Now, when you say high glycemic, you mean any food that you eat that turns quickly into sugar.
RICK JOHNSON [00:22:28] By turns quickly into glucose, and then your glucose levels go up in the blood. And when that happens, it triggers the production of an enzyme that converts some of the glucose to fructose. So the glucose isn’t actually what causes the obesity. It does a little bit through stimulating insulin. The real way high glycemic foods cause obesity and diabetes is because they get converted to fructose in the body.
SHELLEY [00:22:56] You know, Rick Johnson, for a long time there has been debate about whether the body can make fat on its own or it’s only food that you eat that turns into fat. That was the idea 20 years ago. But your thought about this metabolic switch where the body shifts and turns, other energy that’s taken in other food into fat through these pathways is part of this unraveling of a deeper secret to how we get fat.
RICK JOHNSON [00:23:24] Yeah, so let’s just talk about how the fructose works. So fructose is unique among nutrients. Think of energy as two forms of energy. You’ve got the energy that we are burning all the time that we’re using up, and we call that energy ATP. And that energy is in our cells. And it’s allowing me to talk to you right now. It’s allowing you to talk to me. It’s allowing you to stand up and do all the things that you are doing. And it allows me to eat, walk, talk, pre everything. So ATP is our main fuel and we can store fuel. And when we store our energy, it’s in the form of fat or sometimes glycogen. Glycogen is sort of the storage form of carbohydrates, but it’s fat. That’s our main storage fuel.
SHELLEY [00:24:16] Well, that makes sense because it would take a lot of sugar cubes stored on the body to be able to store enough energy. And fat is much more efficient at storing energy.
RICK JOHNSON [00:24:26] Yes, it’s like nine calories per gram. So when you store fat, it’s a great way to store energy. So it turns out that the place where ATP is made are in energy factories that we call mitochondria. And these mitochondria are pouring out the ATP that allows us to do what we want. The mitochondria actually use oxygen to help make this ATP. So much of the oxygen we breathe is used to help make energy that we use. So what fructose does is. Really clever. What it does is it generates a substance called uric acid. And our data suggests that what the uric acid does is it sort of quiets down the mitochondria. It does so by causing oxidative stress to the mitochondria. And when that happens, the mitochondria produce less ATP. And so where does the energy go? If you make less ATP, the energy goes to fat. And so it sort of shuts the calories we’re eating to fat instead of immediate energy.
SHELLEY [00:25:37] You said that it’s not just sugar. It’s not just fructose that can cause this to happen. Unfortunately, this polyol pathway indicates there’s some other foods people eat, especially if this pathway is already running. That will lead to somebody still having problems with their metabolism, with gout, high blood pressure, heart disease, obesity. What are some of the other foods that do this?
RICK JOHNSON [00:26:05] So we’ve already mentioned high glycemic carbs. That’s why a low carb diet is so effective or a keto diet, because it’s removing not only sugar from the diet, but these high glycemic carbs. And when you do that, the fat doesn’t cause obesity because you have to be hungry. You have to lose your ability to regulate your weight. The fructose makes you lose your ability to regulate your weight so that you’re hungry and you’ll keep eating.
SHELLEY [00:26:31] The fructose leads your body to have trouble recognizing where its balance is for health.
RICK JOHNSON [00:26:38] That’s correct. And so the way it does that is it induces a thing called leptin resistance. Leptin is a hormone that’s released by the fat cells that tells us when to stop eating. And normally, animals are very sensitive to leptin and they won’t eat more than they need, and they will just maintain their weight. But in order to gain weight, you have to lose your ability to regulate the way the way fructose does. That is, it causes the body to become resistant to leptin so that when leptin goes up after a meal, it doesn’t tell you that you’re full. And so you end up eating more. And most people who are overweight or obese are resistant to leptin. You know, this was a big discovery years ago that people with obesity don’t respond well to leptin. And you can show that by injecting leptin in people or in animals, and normally you appear censored, selected, and you get an injection of leptin, you’re going to quit eating or reduce your food intake. But if you’re leptin resistant and you get a shot of leptin, you’ll just keep eating. And fructose makes you keep eating once you get left.
SHELLEY [00:27:44] So there’s one camp that would say that the reason that Americans, for instance, have these metabolic challenges and so much obesity, something that they didn’t have 50 years ago as a population, is because food just tastes so darn good. But you describe something where it becomes an addictive, desperate craving. If somebody’s hormonal balance, their metabolism, their fructose signaling is out of whack.
RICK JOHNSON [00:28:13] Yeah, the fructose drops the ATP in the cells, so your immediate energy is less and your stored energy is more. What happens when the ATP levels go down? You sense that low energy and you get hungry, and so you eat more and you become resistant to leptin. And so you’re eating more. Over the last century, the plates of food that people get gets bigger and bigger in the restaurants. And it isn’t because that’s a good thing to attract you. They’re doing it because they know that if they don’t, you’re going to leave hungry. And if you leave hungry, you’re not going to come back. So it turns out that there’s a biology that’s going on and we’re eating more and exercising less because of a switch that’s been activated. And in fact, that switch will drop your metabolic rate, but only while you’re resting. This is important for survival because if you’re trying to survive, you want to be able to forage for food. And so while you’re foraging, you maintain normal energy. But as soon as you quit, your resting energy, metabolism drops.
SHELLEY [00:29:16] Hibernating bear wants to not move very much because it’s hibernating.
RICK JOHNSON [00:29:20] But that’s after I’m talking about when they’re searching for food. So when they’re searching for food, they’re going all over looking for food. They’ll be spending energy then. But to help conserve and to put more fat on for the time when they hibernate, they’ll actually become less active. When they’re resting, when they sleep, they actually sleep more deep. And then the next day they get up and so forth and forage for food. You raise the question of what other foods can do this. This is a discovery that came out of this whole work.
What happened was when we realized that the body can make fructose, we began. And to think about animals in the desert and animals in the oceans, you know, the fattest animal in the world’s the whale. And it’s not eating fruit. It’s not eating bread. So how does it get fat? And so one of the questions was what other mechanisms could drive fat? And the way we tried to figure it out was kind of a pretty cool way. You know, what is the benefit of fat for an animal in this ocean? And here’s the trick. When a whale burns fat or when any animal burns fat, you’re making energy, right? But you’re also making water. So what’s really interesting is fat doesn’t contain water. But when you burn fat, you produce water. You produce water and carbon dioxide. And this has been known since, you know, like the 1900s. Fat is a source of water, not just energy.
SHELLEY [00:30:58] Rick Johnson, you’re implying that one reason that some animals store fat isn’t just for energy, it’s so that they can get fresh water.
RICK JOHNSON [00:31:06] Right. One third of the water that a whale gets comes from its fat.
SHELLEY [00:31:11] And your book was fascinating to read, talking about a desert lizard that makes its tail extremely fat when there’s enough water and food so that during the drought season it can survive and have enough water.
RICK JOHNSON [00:31:27] In hot climates and dry climates. Animals don’t really want to have fat on their body because that can increase their body temperature. So they tend to put the fat in their tails or like on a hump on their back, like the camel. And this way, the fat and the hump can be used to produce water, but it’s not going to overheat them when they’re wandering in the desert. Once we knew that these animals were using fat as a source of water and actually there’s a primate, the fat tailed dwarf lemur.
SHELLEY [00:31:58] That fat tailed part of its name is the clue.
RICK JOHNSON [00:32:00]. Yes, that’s the clue. And what it does is during the dry season, when there’s very little water around, it will effectively hibernate. They call it estimate. It’s like hibernation, but they go into a hollow in the tree and they live off the fat and their tail. And they use it not just for energy, but a key part of it is to get the water from it. So once we knew that fat was a source of water, then we knew that animals would want to put on fat as a means to provide water.
SHELLEY [00:32:31] Rick Johnson You seem to be saying that animals evolved to take advantage of the fact that fat is a stable way to store energy and also to store water.
RICK JOHNSON [00:32:42] Yes, exactly. And this opened up the idea that maybe mild dehydration could be a stimulus for fat, because if you were mildly dehydrated, it would be like an alarm signal to you to say, hey, I might need to find water. And so you would look for water. You could turn on a hormone called vasopressin, which helps concentrate the urine. But couldn’t fat production be also part of this? And so we started studying this and we found that this possible pathway gets turned on in dehydrated state. So if you become dehydrated, your body starts to make fructose to help store fat as a source of water. And then we went on and realized that actually dehydration is not a good condition to be in. The classic dehydration is a situation where you’re losing water like diarrhea, vomiting, like an animal that has bled or something and it’s gotten dehydrated in those circumstances. It’s not really great for the animals. So it would be wiser for the animal to not lose water, but figure out how to gain water. And one way to do that is to eat salt, because if you eat salt, you’re not actually losing any water, but you’re increasing the salt concentration in your blood, which is the same thing that happens when you lose water. But now, when the salt concentration goes up in your blood, that stimulates the paleo pathway. And now when you eat even calves that don’t raise your glucose up, now you’re going to convert those to fructose.
SHELLEY [00:34:24] Oh, because this is a way to get the body to store more fat, which means store more water. That implies you’ve found that if somebody’s eating a lot of salt in their diet can also be increasing their fat storage, increasing a lot of these. Yeah. Parts of the fructose pathway that can be damaging if it’s on too long. Yeah.
RICK JOHNSON [00:34:45] So just like we have a taste receptor to encourage us to eat sugary foods, we have a taste receptor to ask us to eat salty foods. And it’s for the same reason because salt will help us store fat. So it was an evolutionary. Principal to try to get us to store fat. And it turns out that almost everyone who’s overweight or obese tends to be dehydrated. They have slightly higher salt concentrations in their blood. And if you do fancy testing bio impedance, where you measure dehydration through that mechanism, they have a 12 fold increased risk for being dehydrated compared to a lean person. Basically, it’s because of all the salt and also sugar dehydrates as well. And so these two things activate the production of fructose in your body.
SHELLEY [00:35:35] Rick Johnson I’m making the checklist of ideas from your book. Nature wants us to be fat for helping a body be in better balance in this modern world with all of these extra foods that we can eat or substances we can take in. And in the book, you’re suggesting that people might be better off eating less salt, eating less sugar, eating less concentrated fructose, not fruit juice. Correct. Or the table sugars that have a combination of fructose and glucose in them. Also, you mention that if people, when they’re hungry, drink water, they might actually reduce the craving for food at that point.
RICK JOHNSON [00:36:13] Yeah. When we realized that salt could cause obesity and we showed it in animals and we then did clinical studies in people and showed that salt intake correlates with an increased risk for diabetes and things like that. Others have found it to be realized that there was more than one mechanism to drive obesity. Not only sugar, but high salt is playing a role. Interestingly, the way high salt works and actually even the way sugar works partly is by making you appear dehydrated. So when you drink a soft drink, your blood tests will show you get dehydrated, not hydrated. That stimulates the production of fructose to the development of obesity.
SHELLEY [00:36:55] There were some studies some time ago, maybe they weren’t even studies where soda companies tried to get long distance runners to drink sodas, to advertise their product. And the poor runners were so thirsty that they threw the soda cans away just to get regular water.
RICK JOHNSON [00:37:10] Yeah, it’s been shown in experimental studies. Anyway, so we decided that hydrating with water might actually be a mechanism to block obesity. Right. And people have been talking about water intake and drinking 6 to 8 glasses a day. And, you know, all these people run around with their bottles of water and they swear that it makes them healthier. And yet there’s all these physicians that. Right, hey, you don’t need to drink extra water. The kidneys are going to do the work for you. If you don’t drink enough water, the kidneys are going to concentrate the urine. They’re going to take care of you that way.
SHELLEY [00:37:42] It all depends, doesn’t it? Because somebody who is eating in a way that means they’re not triggering this fat switch, survival to switch. They may not need as much water to drink, but somebody whose metabolism is out of balance in this place where their cravings are high, it may be a different story.
RICK JOHNSON [00:37:59] Actually, if you get dehydrated, you’re going to activate the switch. Dehydration activates the switch. So it may be that the kidneys can control the urine output so that your blood volume ends up being normal. But if it’s been activated to try to hold on to water, it’s also been activated to make you fat. That’s the problem. We tested this by taking people and giving them salty soup. What’s great about soup is you can hide the salt in it. And when we gave them salty soup, we could show immediately their blood pressure went up right away and they activated the switch. We could show it, but if you gave it with water, you could block that. And if we took animals on sugar and we gave them extra water, we could reduce their risk for obesity, even if they ate the same amount of sugar. So it turns out a lot of the way this is working is through dehydration.
You know, about ten years ago, it was discovered that people with obesity tend to have a circulating hormone called vasopressin that’s high. And no one understood why people with obesity have this elevation in their hormone called vasopressin. Invasive pressing is the hormone that holds on to water, and it does so by reducing the amount of urine you make or concentrates the urine. It’s what makes the urine dark yellow. And so everyone was thinking, oh, this is what vasopressin does. This is what I learned in medical school. Vasopressin is the hormone that blocks us from losing too much water through the urine. But in some animals, vasopressin has other mechanisms. For example, in the frog, vasopressin prevents water loss through the skin of the frog. And there’s some evidence that vasopressin may actually reduce the loss of water vapor from the lungs. So we thought, well, maybe vasopressin is involved in obesity. Maybe it tries to store fat. And when we studied it, we found that Faisel pressing was in fact. A hormone that drives fat. And that it’s working not to the classical receptor it does for urinary concentration, but it works through a special receptor called the V1 B receptor. And when that happens, pays a press and actually drives fat production. It’s actually part of how sugar causes fat.
SHELLEY [00:40:19] And so all of these are examples where you’re eating food, maybe your body even needs the energy, and instead your cells are shunting the energy, not into something you can use to breathe or move or something like that. But instead your body is shunting more of it into storage as fat. Yes. So you’re saying dehydration all by itself can trigger this so that you’re not using the energy in your body to repair yourselves? You’re using it to turn this energy into fat.
RICK JOHNSON [00:40:50] Yeah. So we talk about hydration. Hydration is good because it will reduce your risk for being fat to be well hydrated. If you’re dehydrated, it’s going to turn on the switch. But there’s a new phrase that’s called under hydrated and under hydrated refers to the fact that you start by being a little thirsty, but you’re able to correct it. So you’re able to hold on to water and kind of turn off this mechanism so you’re no longer thirsty. But what’s happened is your urine still concentrated because everything’s working to keep you in balance. You’re still turning on vasopressin, you’re still turning on the polyol pathway, and you are now hydrated normally, but at the expense that these systems are turned on. So you’re under hydrated. And when that happens, you’re actually triggering the fat production. You think you’re hydrated, but you’re only hydrated so that you’re no longer thirsty. But all the systems to hold on to water are still turned off.
SHELLEY [00:41:54] Well, we have talked about so many different ideas that tie in with what we choose to do, starting with having high concentrated forms of fructose in sodas, in fruit juices, plus foods that are very starchy can end up triggering the same pathway that starts to store fat. How dehydration and salt can both trigger this pathway as well.
RICK JOHNSON [00:42:19] And there’s a third way, too, Shelley.
SHELLEY [00:42:21] These two are big enough, but go on.
RICK JOHNSON [00:42:23] They’re they’re a very big way. So the other thing is we remember we have a third taste. That third taste is called savory. It’s you know why tomato sauce and spaghetti sauce tastes so good? It’s kind of like that cured dried tomatoes taste. That’s why gravies are good. And curing meat makes it delicious. That’s why beer is so good because of the yeast extract. It’s why Caesar salads taste good, you know, because of the parmesan. And it’s why blue cheese dressing tastes good. To some people. The umami flavor is really loved and the umani flavor is due to a substance called glutamate, also to two nucleotides called I am P and amp and sadly I am an amp are directly in the mechanism to generate uric acid. You know, when fructose is metabolized that makes uric acid and it uses these substances that trigger this taste of savory. I amp and amp are part of that pathway. And not only that, glutamate turns out to be converted to uric acid in the body. These three substances can activate the switch as well, and they do so through the same pathway. But just a little bit after the fructose, especially processed red meats tend to be rich in this and things like organ meats and shellfish, beer, they contain some of these substances and they can also make you fat by activating the switch. And the your mommy flavor is basically there to try to attract you to eat these kinds of foods. So it’s a little bit depressing. The good news is the mommy pathway is less powerful because we don’t eat much of it. We only a few grams of glutamate a day, but we eat 70 grams of sugar today. So there’s a big difference in the amount that we’re eating. And sugar is the big boy that’s driving this high. Glycemic carbs are the second big one. But it is true, you can activate this pathway. And, you know, have you ever noticed, Shelly, how people love to drink tomato juice on airplanes? Bloody Marys? Maybe you never knew that, but it’s even in the Internet, they say, you know, why is it that when I fly I like Bloody Marys and things like that? Well, the Bloody Mary has slacks, made a juice that’s rich in glutamate and a little bit of alcohol and stuff like this, which also helps you generate uric acid. And when you do that, it reduces the ATP production and shifts you more to fat storage and. That actually decreases your oxygen needs. So when you go out in a plane and you go to 7000 feet, the oxygen content in the air is just a little bit less. And it’s my belief that that is why the Bloody Mary case so good when you get in an airplane because you’re activating the switch, which has a tendency to reduce your oxygen needs just a little bit.
SHELLEY [00:45:20] Rick Johnson The next time I’m in an airplane, I’m going to order a Bloody Mary.
RICK JOHNSON [00:45:24] Yes. Or 2 minutes or she’ll just see, you know, a lot of people go, I never drink tomato juice or Bloody Marys unless I’m in an airplane.
SHELLEY [00:45:32] But also, from what you’re saying, just don’t do it too often because it can trigger some pathways that now and then to stimulate them and tweak them is fine. But to be stuck in these pathways is really detrimental to health. And people can read your book, Nature wants us to be fat to find out not only all of the details of these mysteries, but also some of the dietary recommendations you have, foods you can eat, ways you can live that will benefit you so that you’re more likely to live a life that has a long health span and be symptom free of some of these terribly painful or die young or be debilitated young diseases.
“Dietary Suggestions from the book, Nature Wants Us to Be Fat”
RICK JOHNSON [00:46:10] And in my book, I actually lay out a plan. And I also believe that you should still be able to eat a little sugar, you should still be able to eat a little bit of high glycemic carbs. And a lot of it is supported by research and experimental studies, including studies where we supplemented patients with with fruits, for example, and showed that natural fruits, when given modestly, actually makes things better, not worse. So please don’t hear this talk and go, Oh my God, I can’t eat anything that’s good, because it’s not true. It’s the problem of eating some foods that are really bad. Like liquid sugar is really bad. Once you understand the mechanism, you can actually figure out the best way to avoid activating this switch and giving you back your help.
SHELLEY [00:47:00] Now, I was promised 15 minutes, actually, half an hour, but 15 minutes to my own questions.
RICK JOHNSON [00:47:05] Yes, sure.
SHELLEY [00:47:07] So the first one that I have is, before creatures evolved to store fat on purpose and for beneficial purposes . . . What was the survival advantage of converting fructose to fat?
RICK JOHNSON [00:47:18] The advantage of converting fructose to fat has always been helping survive, to provide another source of energy when you don’t have food around.
SHELLEY [00:47:27] Was that the earliest reason for that? For single celled creatures, are there single celled creatures that don’t store fat or that evolved to store fat? And what was the first reason they did it?
RICK JOHNSON [00:47:38] I’m not aware of single celled creatures storing fat that does not involve, from my studies . . . anything that’s storing fat. It tends to be using an aspect of this pathway.
SHELLEY [00:47:51] How about algae? Does algae have this pathway? Algae makes fat and it’s a single celled creature or thing.
RICK JOHNSON [00:47:58] I do not know. I can’t answer that question. But I do think that this pathway has a basis that goes way back in biology.
SHELLEY [00:48:06] It’s a pathway that some animals have taken more advantage of than others. It is intriguingly consistent. But if we step back from that and see what was happening before, what was the reason that these creatures did this?
RICK JOHNSON [00:48:20] So if you go back to the very, very beginning of life. Okay. We’re going to go way, way, way back. The earliest life was thought to just be RNA. They called the RNA world and there was no DNA. There was no proteins. If you were an organism with RNA and the RNA starts to degrade, what you generate is uric acid. So it’s like a degradation product. And so one might consider the possibility that it could become a signaling mechanism because you don’t want to have your RNA degraded. So if you’re an RNA form, uric acid was probably an alarm signal for degradation of the RNA. Today we are in a world has carried over to current life and some of the most important components of RNA are involved in the biology of life. So ATP, for example, the essence of energy, is ab RNA carryover, uric acid is an RNA carryover. When it’s cell alarm signal, things like Nad H and these very important mediators and the biologic reactions in the body are all carryovers from the RNA world.
SHELLEY [00:49:31] So your guess is that it has something to do with RNA which connects with uric acid?
RICK JOHNSON [00:49:36] Uric acid turns out to be a survival mechanism for many, many animals, and has a very basic role in both survival and reproduction. If you’re, for example, a crayfish, you use uric acid to help you survive in brackish waters because it helps decrease your oxygen needs. If you’re a flatworm and you are mating, you use uric acid as your pheromone to tell the other worm that you’re ready to copulate. So uric acid was developed as an alarm signal to help animals and even in bacteria. Uric acid is used as a survival mechanism in the setting of radiation or high heat. So I think that very early on, uric acid took on a role of being a survival or alarm signal.
SHELLEY [00:50:28] A signal because it was something that was excreted by an organism.
RICK JOHNSON [00:50:32] It was something that was broken down. So when you’re RNA or DNA or ATP is broken down, this is generated. So it sort of says, hey, what’s going on? Are we losing our genes? Are we losing our RNA? Are we losing our energy? So it becomes like an alarm signal.
SHELLEY [00:50:50] ((EXPANDED EXPLANATION)) It seems to me that sometimes when someone finds a reason that’s partway through the evolutionary channel, there may be another reason further back in time that still is there sometimes, and it’s still remains a reason that things happen. I’m not an expert on evolution, and what I say next will probably make an evolutionary scientist scream. Forgive me. Here it goes: The simple example that I think of is shellfish. Shellfish did not evolve to have a shell that opens and closes because long ago, a mollusk without a shell said, “Someday I’d like to have a shell.” Instead, before a shellfish was even a blob without a shell, way earlier in its evolution, it was a single cell, and it was excreting calcium because calcium signaling requires that you have to be spitting out calcium to keep calcium signaling clear inside the cell. That works fine for a single celled creature, and it maybe works for a creature that can move away from where it’s been spitting out calcium. But in mollusks, when the cells got together as a multicellular creature, they evolved to specialize in hanging out in one place where they slurped nutrients out of the ocean. This meant a lot of calcium flowing in and out of them, and perhaps the calcium often built up around them. Eons ago, a lot of those evolving mollusk like creatures probably died by being smothered in their own calcium excretions. Then at some point, by accident or intent or whatever, some mollusks evolved to organize the mounds of calcium into a protective shell. So the calcium that might have smothered them because the calcium that was their fortress. So it wasn’t that the mollusks thought that they would need a shell some time in the far future. And the original purpose of calcium excretion wasn’t to ultimately evolve to make a shell. Originally, those mollusky-things were spitting out calcium to keep signaling in their cells clear. And then later on, they programmed in an evolutionary drive to make shells out of the calcium they excrete. So it was a good evolutionary “invention.” But the drive to make shells out of the calcium . . . that’s not the main reason they excrete calcium. Deeper down in time, those shellfish needed to excrete calcium to keep their signaling pathways clear. And even today, even though making shells is important, it’s probably MORE important for a shellfish to spit out calcium to keep calcium signaling inside each cell clear. That’s still probably more important for these shellfish than the need to make a shell. So . . . how about humans who store a lot of fat — is there something about getting the volatile sugar energy out of a cell that means it’s important to sequester the energy in the more stable form of fat? Is there something about that which is still at play, even in animals like bears who very intentionally store loads of fat because they hibernate? END OF EXPANDED EXPLANATION WHICH WAS NOT PART OF THE ORIGINAL INTERVIEW))
RICK JOHNSON [00:51:55] You know, there are mutations that change things. If this shellfish, this mollusk is spitting out calcium and it takes mutation that allows it to start forming the shell, perhaps that helped it evade a predator. And then it survives. And then it passes that mutated gene to another mollusks.
SHELLEY [00:52:21] And then at that point, it becomes a gene for expressing and creating a shell because the shell has survival advantage. But it didn’t start that way.
RICK JOHNSON [00:52:30] It starts as a random mutation. You know, it’s not like nature wants us to be fat. It’s the fact that in the process of evolution, we develop these protective mechanisms.
SHELLEY [00:52:43] Was it that initially, though? And that’s what I’m curious about, because you’ve done so much to delve into this. I’m curious about this other part. ((FURTHER EXPANDED EXPLANATION — What if the original reason for storing fat in a cell was to take a volatile and unstable form of energy — a sugar, and make it into a more stable form of energy without going to the effort to absolutely spit that energy out yet?)) This may be off base, but one example I could point to is a scientist named, Matthias Heineman, who was looking at the thermodynamics of Why Do Yeast Make ethanol. Why do they spit out this perfectly good sugar energy that they’ve been consuming? ((And they do it halfway through the process of turning that ethanol into usable energy))
RICK JOHNSON [00:53:14] Well, ethanol in the early days, animals couldn’t really eat ethanol. And so it was a way to avoid an animal from eating the yeast. And actually, I’ve done a little work on this.
SHELLEY [00:53:28] That was a benefit of (ethanol excretion), but that was not the original reason that they spit it out.
RICK JOHNSON [00:53:32] The thought is it always begins as a random mutation, and then if there’s a survival advantage, then it stays, it gets passed to the next lineage.
SHELLEY [00:53:41] But Heineman would say that the random mutation was that if a yeast is taking in sugars too fast, then it starts to cause an inefficiency in the middle of the ((metabolic)) pathways, which is toxic. And that toxic inefficiency in the middle ((builds up)) where if it just kept trying to make the sugar that’s being metabolized into ethanol and push onto other things, if it just kept doing that and made the assembly line ((of its metabolism)) do that, it would back up so much ethanol, it would be toxic to the yeast and kill it. And so his hypothesis is that there’s something called the Gibbs equation of thermodynamic whatever. And it’s that at a certain point that little yeast cell figures out that this is too much to handle right now. And if it tries to keep going, it’s going to expend more energy than the effort is worth. And in the meantime, it will have to deal with a buildup of this toxic product and it’ll kill the yeast.
ALCOHOLISM AND THE POLYOL PATHWAY
RICK JOHNSON [00:54:50] Well, I have to say, I’m kind of Darwinian, so the way I view it is that when a mutation occurs, if there’s a natural selection advantage, then that mutation may be accepted and end up then passed into the system. So let me tell you my yeast story. Alcohol story. Our ancestors were not able to drink alcohol, but it could be at about around 10 million years ago, a mutation occurred that allowed our ancestors. They weren’t human then. They were kind of pre-human that allowed them to drink alcohol. It was during a period of famines. Our ancestors were still primarily eating fruit as their favorite food when the fruit trees became more and more sparse. A lot of the fruit they would find might be have already fallen but be fermenting. And so they were not edible. And what we think is that this mutation that occurred allowed the animals to eat the fermenting fruit and to metabolize the alcohol and thereby get some of the sugar that was present in the fruit to help them survive so that it was a survival advantage to have that mutation. But the consequence is that now they can metabolize alcohol. And so not too long after that, alcohol becomes, you know, something that people enjoy and like. And one of the interesting things is alcohol activates the polyol pathway, too. So it’s another way to stimulate sweetness. And in fact, when we were able to show that the craving of alcohol can be blocked by blocking the craving of sugar, that the two are intertwined. And I actually have research funds from the National Institutes of Health to try to develop inhibitors of sugar craving that will also block alcohol craving. So the two are definitely linked.
SHELLEY [00:56:51] From what you said about what people eat. If somebody who has a propensity toward alcoholism drinks enough and avoids sugars and salt and stuff and modifies what they eat, they may not have as much alcohol craving.
RICK JOHNSON [00:57:07] Alcohol craving and sugar craving are linked. And if you stop drinking alcohol, people will tend to want to drink sugar or eat sugar. And if you take people who crave sugar and take away their sugar, they may end up wanting more alcohol.
SHELLEY [00:57:23] That’s right. At AA meetings, the amount of candy is huge.
RICK JOHNSON [00:57:28] Probably. I’ve never been to an AA meeting, but I bet you it is. But I will tell you this as a physician, when I have a patient get admitted for alcoholic liver disease and I go in to see them, there’s usually a soft drink can on the table and both can cause liver disease. In fact, in our animals and we block sugar, fructose metabolism, we can block alcohol induced liver disease. So we actually believe that the liver disease from alcohol is really a sugar disorder. So the two are really linked.
SHELLEY [00:58:04] That was fascinating. I had I had thought that alcoholism had something to do with the P 54 pathway, but my colleague Beth Bennett set me straight. Okay. So it is more it’s a mystery and it’s something where it’s one of these parts of the body that tends to wear out and be out of balance the more that somebody is exposed to this stuff. Yeah, yeah. Lots of things like that.
RICK JOHNSON [00:58:37] This can go really deep
KIDS AND ENERGY AND MITOCHONDRIA
SHELLEY [00:58:41] And, and there’s, there’s some things I disagree with in your book.
RICK JOHNSON [00:58:45] Oh, okay. What do you disagree with?
SHELLEY [00:58:49] Well, you said that one reason that children don’t have these metabolic challenges is because they’re more inefficient at processing the things that lead to fat storage.
RICK JOHNSON [00:59:03] We did a study right here at Children’s. So we took children. You know, fructose is absorbed through a transporter called Glut 5. Glut 5 in a normal animal, Very, very little else in the intestine. So if you give fructose to a person who’s not ever had sugar, they’re going to get cramps and diarrhea because they can’t absorb it. And then over time, as you give them more and more sugar, they turn on these transporters so they can absorb it better. And you can show that in animals easily.
SHELLEY [00:59:35] Oh, this is diarrhea.
RICK JOHNSON [00:59:36] Not diarrhea. I’m talking about absorption of sugar. If I give a load of fructose to a five year old who’s never had sugar.
SHELLEY [00:59:44] That was a rare five year old.
RICK JOHNSON [00:59:45] Yes. In this country. Yeah. So if you give fructose to a five year old in this country who’s had a lot of sugar, it will absorb more than if they had never had sugar because they have the transporter. So we did a study at Children’s where we took kids that were lean, kids that were overweight, and kids that were obese, with fatty liver documented by biopsy. We give them all the same dose of fructose. We measured how much they absorb and all the overweight fat kids with fatty liver. they absorbed all their fructose. People that were overweight had intermediate absorption and the people who were lean had really reduced absorption. So the same amount of sugar it goes in, but not the same amount is absorbed.
SHELLEY [01:00:32] Well, I’ve been around some little kids who after they eat a cookie, it’s like being next to an oven. Their body is burning off the sugar. They’re not getting fat off of the sugar. Instead, their bodies are like an oven that’s just flaming. You can sit next to them, and you’re warm.
RICK JOHNSON [01:00:54] It’s thermogenic. The rapid burning of fructose.
SHELLEY [01:00:58] Is that inefficient or is that effective? Is that child’s body being effective at not being overwhelmed by a substance that is too much for it?
RICK JOHNSON [01:01:08] No. What happens is they’re burning . . .. The ATP levels are falling and they get hyperactive. And then after that, they’ll actually reduce their energy. They’ve activated the switch.
SHELLEY [01:01:24] You know, it’s easier for me to have fat on my body today than it was ten years ago. Is that because my body has finally become efficient at storing fat, or is it because my body is less efficient at being able to cast off excess energy? Would keeping the excess energy within my body be just as hard on my body as it would be for the yeast to use all of the glucose that goes in, instead of sptting out as ethanol.
RICK JOHNSON [01:01:50] There’s multiple reasons for why when a person is young, they tend to be invincible. And then when you get older, your metabolism slows down and you become overweight easier. When you’re young, you tend to have a very healthy mitochondria. Your energy factories are really healthy. Takes a while to dampen them down. Also, the ability to absorb sugar is is reduced in the beginning, but that’s not the main reason. We tend to have a very healthy mitochondria is what kind of keeps you going. And what happens is the way this ((Polyol)) pathway works, it causes oxidative stress to the mitochondria. Each time that happens, the ATP production goes down, the fat storage goes up, but it’s transient and then everything goes back to normal. But when you keep hitting with oxidative stress over time, the mitochondria take a beating and over time they start to decrease in number.
SHELLEY [01:02:49] They get sluggish and they get senescent.
RICK JOHNSON [01:02:51] They get senescent, they fission. The amount of ATP produced stays down.
SHELLEY [01:02:55] They cause more pollution.
RICK JOHNSON [01:02:57] Once the mitochondria are low, then what happens is it’s very hard to lose weight because you’re kind of like reset to that. Higher weight. So you can lose weight, but you’ll want to go right back to that weight. The end of my book, I talk about this and I talk about how you can reverse that. That’s the whole bit about exercising in zone two and stimulating mitochondrial growth and all that.
SHELLEY [01:03:24] With a kid who is obese in your studies, is that kid’s mitochondria more efficient or less efficient than the child who is lean?
RICK JOHNSON [01:03:34] Oh, they’re less efficient. The child who’s obese is less efficient, but oftentimes their mitochondria numbers are still normal. So when you first become overweight or obese, usually the mitochondrial density is still good. Your energy levels, your ATP levels tend to still be pretty good when you’re not eating sugar. Obesity is much more reversible in that very beginning. If you find someone who’s only been overweight or obese for like five years, it’s much easier to cure obesity than if they’ve been obese for 20 years because at that point they’ve lost more of their mitochondrial energy. The longer you’ve been obese, the harder it is to fix it.
SHELLEY [01:04:15] Still thinks it’s fixable?.
RICK JOHNSON [01:04:16] This is the incredible thing. It’s still fixable. My friend Inigo San Millan. he’s the man who’s really done a lot of wonderful work on restoration of the mitochondria. You might want to talk to him because he’s really like the world’s expert and he’s here in the Denver area.
SHELLEY [01:04:37] I have enjoyed talking with you about this and hearing what you’re doing. This one question I have. Well, we’re not quite seeing it the same way as a question, but I do think you’re on to something. And I do think that there may be something driving fat storage beyond storing energy, in evolution earlier, that will be interesting to discover.
RICK JOHNSON [01:05:00] It comes down to uric acid, I think is the key.
Podcast: Play in new window | Download (Duration: 1:06:15 — 91.0MB)
Subscribe: RSS
Here’s the Extended Version of the Interview with Russell Castagnaro about Colorado’s official way to display your vaccination record AND your driver’s license, on your smart phone. – Shelley Schlender
Podcast: Play in new window | Download (Duration: 15:48 — 14.5MB)
Subscribe: RSS
Overview: Foodborne Salmonella infections MIGHT pave the way for arthritis, Parkinson’s disease, Alzheimer’s and ALS, according to a new study about the potential long-term effects of a salmonella infection. Symptoms of salmonella infection can include fever, abdominal cramps and diarrhea. Healthy people usually get over a salmonella infection after about a week. But sometimes, people later develop creaky joints and pain — you know, arthritis. Why a brief gut infection can lead to long term arthritis has been a mystery. The new study documents how the inflammation of joints and other symptoms of reactive arthritis may involve curly “curli” proteins that cover a salmonella bacteria. These curli proteins can stick together like velcro, to produce a biofilm. Even after our bodies vanquish a salmonella infection, biofilms can remain in body tissues. If the immune system keeps attacking the biofilms, it can inflame our tissues and hurt them. For more, here’s one of the lead researchers on the new paper. He’s Aaron White from the University of Saskatchewan School of Medicine. White is Chair of Biotechnology at the School of Medicine.
Aaron White: So this study came about because Cagla Tukel is at Temple University. She had studied the Curlii protein itself and showed that if you injected into an animal, you get auto immune responses.
Shelley Schlender So there’s just a lot even in that one sentence, that is fascinating. Let’s start out with the body of a bacteria. I’ve always pictured a bacteria as this teeny tiny thing that looks kind of like a gel cap. You know, it’s just this blob that is kind of smooth on the outside, but in reality it has these proteins that stick out that look a little bit like fusilli noodles. They’re kind of curly.
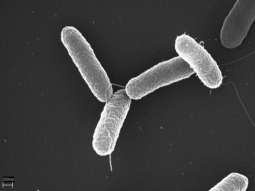
[Yeah. The organisms that a lot of people study in the laboratory are different than the wild type ones. So the ones in the wild are covered in these, like you say, fusilli or pasta-(shaped proteins). Their surfaces are very complex, adorned with proteins and sugars, things that enable them to interact with their world. Like with our immune system, for example.
Shelley Schlender These little bacteria are not just smooth on the outside. They have what could be antennas. They could have channels coming in. To the naked eye, under a microscope, it looks like they’re furry. It looks like they’ve got curly hair.
Aaron White That’s very accurate. I’ve been studying what they do for salmonella, enable the cells to stick together. And in the past, we had thought that that only happens kind of outside of an animal or outside of a human like as a way to survive in the environment. (SS COMMENT: In other words, when the diarrhea caused by salmonella causes the microbes to be expelled back into the world, a curli biofilm helps them survive heat, UV rays from the sun, drying out, etc etc during them time they’re on the ground, in the water, on the surface of a fruit, etc. The biofilms give the salmonella a way to survive the part of their life cycle when they’re out in the world, waiting for next next time they can will be eaten and enter a new digestive tract and go through their life cycle once again.)

Shelley Schlender OK, we’re going to get back to how this is involved with creaky joints and maybe Alzheimer’s, maybe other autoimmune conditions like lupus and Parkinson’s disease. But it starts with the fact that these bacteria have this kind of furry curly outside that lets them stick together like Velcro to make something called a biofilm.
Aaron White Yeah, biofilm is a large group of cells that are stuck together and it provides a survival advantage for the bacteria. So they survive better as a group than they do as an individual.
Shelley Schlender: Does that mean that when there’s a biofilm with a lot of microbes hanging out together, bacteria in this case, they’re harder for invaders to find? They’re protected from the elements. What does the biofilm do for the bacteria?

Aaron White So that’s been a major focus of my research, is the function of biofilms. Imagine the bacteria ends up in a situation where it’s very dry. There’s no nutrients. Right? If it was this individual cell, it would be very fragile. But as a group, as a biofilm, they cover themselves in this protective coating. And that’s what Curli is part of.
Shelley Schlender Excuse me. I’m hearing a lot of beeps of e-mail.
Aaron White: You know what that is? Twitter! Because I just joined Twitter. It’s beeping at me.
Shelley Schlender: Is it beeping at you about your article?
Aaron White: Yes.
Shelley Schlender: Oh, my gosh.
Aaron White: Scientists that I know that have been on Twitter for ages. Congratulations. Or people I don’t know.
Shelley Schlender: They’re literally all atwitter about your new study.
Aaron White Yes.
Shelley Schlender So biofilms are in nature. It’s a little bit like these bacteria form a union or they form a co-operative, so that if it’s too dry, if it’s too hot, they can shelter themselves a little bit by combining together.
Aaron White: Yes, you can think of it as nature’s way to survive better. Many, many bacteria do that.
Shelley Schlender: And they’re not a multicellular animal like a mouse or a frog or us. But it gives them some advantages of cells sticking together. How about the biofilm, the bacteria on the outside? Do they sacrifice their lives?
Aaron White: There is a bit of that. Originally when we studied this, we thought how ants come together and cross the stream. They make sort of an ant raft. We thought of that for biofilms in these bacterial cells. There is some aspect, it seems like, of cooperation, but it’s all aimed at survival, to better withstand stresses. Basically, the cells themselves, too, in the biofilm are more stress resistant than individual cells would be if they weren’t in a biofilm.
Shelley Schlender: And so all of that, Aaron White, is happening out in the world, like in ponds, on the surfaces of rocks, in soil. There are biofilms.
Shelley Schlender: There has been talk among health care professionals and scientists for a long time that sometimes biofilms can form inside of us.
Aaron White You know, in our lungs, in our mouths, even in our digestive tract. Bacteria do need biofilms to help them survive too. You know, when you get a medical device or a catheter put in? Certain bacteria, It’s very accepted and known that they form biofilms on medical devices in your body, artificial joints. That’s a huge problem. Bacteria forming biofilms on the surfaces.
Shelley Schlender Ewww!! it sounds like these things end up with biofilm slime.
Aaron White Yes, it’s very accurate. They’re very hard to treat with antibiotics. Much harder than the individual cells are. They become a major problem. Doctors have known for many years, 50 years, that the ability of bacteria to stick together makes them more resistant to treatment. They’re associated with hospital acquired infections, those kind of things.
Shelley Schlender OK, so we know that biofilms can be inside of people. And when they’re inside of people, does it make it harder for us to detect that the microbe is there or does it just make it harder for us to wipe it out?
Aaron White Harder to wipe it out. You can detect them fairly easily in some case because they’re accumulating greater numbers than they would just as individual cells. But they’re hard to treat.
Shelley Schlender: Is it like they put a layer of Saran Wrap on themselves or a skin?
Aaron White: Tougher. Concrete.
Shelley Schlender: Concrete? So these biofilms end up with kind of a concrete layer on themselves?
Aaron White: Yeah. That’s what’s unique about Curli. They’re incredibly tough, resistant proteins. Hard for your body to break down.
Shelley Schlender: There’s another complication with these. Our bodies make something like Curli.
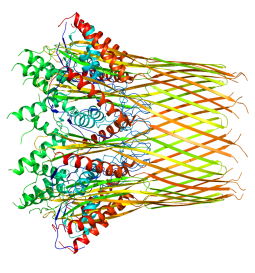
Aaron White This is a complex area to explain. What is unique and what we come to appreciate about Curli is that they’re a protein called an amyloid.
Shelley Schlender Oh, I know that term amyloid.
Aaron White Right. It’s is a very characteristic three dimensional structure.
Shelley Schlender That word amyloid comes up with Alzheimer’s disease especially.
Aaron White Yeah, and that was sort of the scary part of our research, really was realizing, through reading the literature and other papers that were published fairly recently, that Curli shares the same three dimensional structure as the amyloid plaques that form in Alzheimer’s disease.
Shelley Schlender Those amyloid plaques in Alzheimer’s disease. There’s been a longtime debate about whether those cause Alzheimer’s or they’re a sign that there’s been brain degradation. Whichever one it is, when they’re present in high numbers, it’s more likely that there’s been brain damage.
Aaron White I don’t claim to be an expert about Alzheimer’s disease. I’m learning about it. So it’s my understanding that these plaques, when they’re in the brain, they sort of cause dysfunction in the brain.
Shelley Schlender There’s the debate about whether or not the amyloid actually generates dysfunction or whether they’re a bandaid that the body puts in as a structure to keep damage from cascading. So there’s lots of questions about it. But there’s no doubt that the amyloid itself is a sign that there’s been stress inside the brain.
Aaron White Right.
Shelley Schlender Our bodies make amyloid. So not just bacteria. Our bodies make this structure that is very similar to the one in the curli proteins in microbes.
Aaron White: The difference is that the human proteins that become amyloids have a normal function, that’s not an amyloid. It’s just that they mis-fold and make these amyloids.

Shelley Schlender I’m going to stop again then, because you just said something else, that the proteins that we call amyloids that are associated with Alzheimer’s disease. We know that they’re a mis-folded protein. There’s something about them is folding that may make it cascade, meaning more and more get made.
Aaron White 7The scary part is how similar the three dimensional structure of curli is compared to these amyloids that are caused by mis-folded human proteins. Scientists, doctors have wondered how these human proteins start to mis-fold and how that process is speeded up. And that’s where the connection to our works comes in.
Shelley Schlender 8:16] OK, so strangely folded curli proteins on a microbe are a good thing for the microbe. It’s a good thing because it helps them stick together and make a skin and protect themselves from all kinds of things. However, the properly folded protein in the microbe looks very much like a protein looks inside of a human when it’s mis-folded and starting to do some things that are associated with a lot of damage.
Aaron White: That’s exactly it. What was so surprising about our paper, why it was such a big discovery is that these biofilms were thought to be outside the body only. So to actually discover some of these things inside the body means there is a greater chance for interactions to occur between these curli proteins and these human proteins which mis-fold.
Shelley Schlender n the case of your study, you weren’t studying what’s happening inside of a human body. You were studying what’s happening inside of the body of a mouse. But it was with these curli proteins that came from salmonella. Is salmonella unique in making a curli protein that is very similar to the mis-folded amyloid in human bodies, or are there other bacteria and microbes that can make this furry outer stuff that ends up looking very much like an amyloid, that’s mis-folded in a human?
Aaron White I guess what what I mean is, maybe scary is the wrong term. But I mean, what makes this more of a generalized, wide scale thing is that Escherichia Coli, So E. coli, the most commonly studied bacterium in history, also makes curli. In their intestines, most people have E. coli. I’m not saying that they do made curli, but they have the ability to do it. Plus, there’s other members in normal bacteria that can make curli as well.
Shelley Schlender: All right. So there’s a fair number of microbes that can make this furry curli outer coating that can look very similar to the mis-folded amyloids that doctors find in the brains of people with Alzheimer’s when they do autopsies. You’ve used this the word scary. Let’s stick with that, Aaron, White, there in Saskatchewan. .
Aaron White: (LAUGHS).
Shelley Schlender: Let’s stick with that word, because are you implying that you started wondering what if a load of these microbes with these curli proteins, if they get into the body too much? What if they do something to how our immune system works, or how our own protein folding works, so that our good proteins say, Hey! Let’s take an idea from these mis-folded proteins and let’s do that, too!
Aaron White: Yeah, that’s exactly what there’s a potential for. We end up eating in our diet. A lot of these bacterial amyloids. If your intestine in your gut is functioning normally, those amyloids never get exposed to anything in our body other than the digestive tract. And the same thing goes for the auto immune responses that we noted in response to Curli. That seems to only happen once the lining of the intestine is breached.
Shelley Schlender: Well, then you’re telling us, even though there’s some scary implications to this, this has been happening for millions of years in mammals. And usually it works out OK because our digestive tract keeps the curli proteins from filtering into our blood.
Aaron White: Well, into the tissue surrounding the intestine and then, I guess, ultimately to blood. But as scientists, we tend to think of it as more into what we call the systemic tissues, so the tissues that are outside the intestine.

Shelley Schlender That’s good news, but also not good news because there is a condition that’s been talked about for decades now called Leaky Gut. (SS COMMENT. Go to Leaky Gut Medical Sceptics for an overview about why medical groups have said a “leaky gut” is quack science. Go to Loren Cordain founder of the Paleo Diet, for a viewpoint about Leaky Gut being a real issue for many people.) A more specific term for leaky gut is intestinal permeability , where proteins from our food don’t get digested into small enough teeny tiny pieces and instead find some cracks to get through that are bigger, and so larger fragments of proteins can get into our other tissues, outside of our digestive tract. You’re nodding as we’re talking.

Aaron White: You’re absolutely right. So that’s a problem. It just gives a greater chance that there’s interactions between, quote unquote, bad proteins and human proteins. That’s what was surprising to us in this paper that we published. First of all, that we could detect salmonella biofilms in the gut, but that we know salmonella during its normal infection, like food-born illness, causes mass inflammation in your gut. And that creates sort of a leaky gut syndrome, for a time period, until salmonella is cleared. But during that time, we know that these biofilms are then there, and that the curli proteins are there, and the gut becomes more permeable. And suddenly you have a situation where these curli proteins could easily be leaking out into the tissue surrounding the intestine.

Dr. Tukel has studied for years now, what happens when you inject Curli into a body and it causes autoimmunity? And so we teamed up because my specialty really is on the biofilms and detection of Curli. She had a lot of evidence that salmonella made biofilms in the body, but she’d never been able to detect it directly. And that’s where I came in and helped to detect it. And so now all the things that she had measured in previous years, we learned could happen in the course of kind of a natural salmonella infection. The biofilms were there, plus curli proteins cause these autoimmune reactions. In this case, arthritis, which is again, a surprise.
Shelley Schlender: Let’s hold onto the fact that you have said that the good news is that a healthy gut that is not leaky is likely to keep these microbes and their curli proteins from going into the bloodstream.
Aaron White: Yeah. And it makes sense from a historical perspective that if our bodies reacted to every amyloid protein we saw, it would be hard to survive. You’re right. It is comforting. And that was, for me, a quite an interesting part of this paper. If the gut is intact and functioning normally, they even restrict the access of these type of proteins to the outside.
Shelley Schlender: I’m going to give my gut a little pat right now. It’s amazing some of the things her digestion does for us and the reasons to help it be healthy. There has been some thought among some health researchers and maybe some scientists too, or both, that some of the modern practices of how we live do more to mean that there’s cracks in the gut, meaning that more things leak out. There’s foods that people can eat that will mean that the gut is not in as good a repair. There are medications people can take that can mean that the gut tends to have more leaks to it. There’s the stress of pollution. There’s the stress of just stress or not getting exercise. All of these things can affect how healthy the gut is. And there is a rise of autoimmune conditions. And it looks like possibly conditions like Alzheimer’s, that may have some relationship to how healthy the gut is. Are you shaking your head going? Yeah, I’m listening to you. Or are you shaking your head going? I agree.
Aaron White: So to put it put this in perspective. And I’ve thought about this for maybe the last six months, to a year, as our paper’s in different stages of getting reviewed and then published, you probably couldn’t pick a worse protein from salmonella to be inside your body. Imagine why salmonella makes them in the first place? It’s to stick together and prevent themselves from getting wiped out. So now you’ve got that protein potentially leaking into the tissues surrounding your intestine. And they’re really, really tough. They’re really hard for the body to clear. In terms of arthritis, maybe these curli proteins can lodge into joints and things like that. And because they’re so resistant and tough, the body doesn’t clear them fast.
Shelley Schlender All right. So they’re hard to scrub away. I keep wanting to have a Brillo pad somewhere inside my body.
Aaron White: That’s very accurate way to to think about it. I 100 hundred percent agree with that. That’s the way I think about it, too. If you could scrub them away! Bacteria making a biofilm to stick together and make themselves hard to eliminate. So Curli is part of that.
Shelley Schlender Is there a possibility that our bodies, when they’re healthy, do have the ability to do good housekeeping and scrub away some of these biofilms on their own?
Aaron White: Yes, very much. And we probably encounter biofilms every day. Why it’s significant with salmonella is that salmonella has mechanisms to disrupt normal gut function, so they can make greater numbers of themselves. So they sort of disrupt the gut and then take advantage of it at the same time. Even if your immune system is perfectly healthy, salmonella has ways to disrupt that.
Shelley Schlender: Other bacteria do as well.
Aaron White: Yes.
Shelley Schlender: And when they do that, that means that the gut can be leakier. More stuff can get out. We can’t really hate these microbes, because they’re just trying to get after our hydrogen. They’re just hungry.
Aaron White: Yeah. Exactly. It’s their life cycle. They invade us. And then salmonella case, food borne illness, pass back out into the environment to infect other animals, other people.
Shelley Schlender: They’re trying to survive.
Aaron White: Yep.
Shelley Schlender: When our bodies are in good enough balance, a little of them survive, but not too many. But we want our bodies to survive.
Aaron White: Yes.
Shelley Schlender; We want to do what we can to minimize the damage they do inside of us. The problem isn’t just that it’s a curli protein. It’s that there’s often a bacteria coming out with it that’s colonizing some place. And then the Curli protein skin makes it hard to scrub away. Or concrete, as you say, the concrete of the curli protein makes a biofilm that’s hard to scrub away. But the body can scrub it away, if it doesn’t have too many other jobs it’s doing it once. You think?
AARON WHITE: “(Curli proteins) can go into the tissue surrounding your intestine and perhaps lodge away for months. Right? To joints. Your immune system does recognize curli and react to it. That’s the problem, because they’re such resistant proteins that could persist in your body and then you get an immune response to them.”
Aaron White: Yep, I think that’s accurate. I think the curli proteins, once they’re made, the bacteria, doesn’t necessarily have to be there anymore for them to cause problems, because they’re just so resistant. So they can go into the tissue surrounding your intestine and perhaps lodge away for months. Right? To joints. Your immune system does recognize curli and react to it. That’s the problem, because they’re such resistant proteins that could persist in your body and then you get an immune response to them.
Shelley Schlender: That’s another layer of all of this, because now we’re talking about something called autoimmunity. (SS COMMENT: Actually, he’s not talking about autoimmunity yet. He’s talking about hyperactive immunity, where the effort to clear out the curli proteins causes a lot of collateral damage in surrounding tissue. ie, “friendly fire.”). Even after the bacterial infection is killed, are you saying that our bodies can start to say, oh, my gosh, if we see a Curli protein, we need to fight it! We need to get rid of it! Even if there isn’t a bacteria underneath it.
Aaron White: They work through something called the innate immune system.
Shelley Schlender: That innate means that it’s part of the immune system that doesn’t need any training. It just goes, uh-oh, that’s a bad guy. Let’s get it out.
Aaron White: Exactly. As part of our innate immune system, they recognize certain things that they know are foreign or from the pathogen and they react to them. So this is, again, research done by a Cagla Tukel showing that these curli proteins actually bind to bacterial DNA. And it’s the two of them in complex together that really alarms the innate immune system and causes autoimmunity.
Shelley Schlender: Isn’t it amazing that our bodies can tell that a little tiny thing, teeny, tiny, is not supposed to be in our body? And try to get it out of there. That part’s good. Except for two problems. Immune cell warriors have to push their way in to try to get rid of the bad guy. And when they do that, they can damage the healthy human cells around it, as an example.

Aaron White: Yeah. And that’s one of the major things we found in this paper is this inflammatory arthritis. The problem on the joints is the immune response to the bacterial protein that’s there causing inflammation in the joints and then pain. Friendly fire, like you said.
Shelley Schlender: Yeah. And so somebody who’s had a salmonella infection or a bad bout of diarrhea as an example. And then two weeks later, goes, gosh, my joints hurt.

Aaron White: Yeah. There’s a certain number of people that have salmonella infections or other food borne illness do end up with this long term condition of inflammatory arthritis. And scientists and again, doctors have maybe assumed that that was related to the bacteria. But again, in many cases, they can’t detect the bacteria in the body anymore. So then it becomes sort of a mystery. And that’s where maybe Curli can fill in some of the gaps there because it’s such a resistant protein. It’s possible it could be in your body. It persists for months. Perhaps it could explain inflammatory arthritis.
Shelley Schlender: All right. So it could be that even if the bacteria is gone and the doctor looks at someone and says, “I’m sorry, but there’s no evidence that you have an infection. So maybe that pain is all in your head.” Actually, maybe the pain has something to do with the body still fighting the curli proteins.
Aaron White: Yes. That potentially leaked out from the intestine into the surrounding tissues, eventually perhaps reaching a point near a joint. And, yes, the immune system responding to that. That’s exactly right.
Shelley Schlender: All right. And as we’re telling this story, that is somewhat scary. It’s also possible that if a person hypothetically could pull out enough stress from the body and let the body go through a full healing process, that the body could get rid of the curli proteins and heal, and the pain potentially might go away.
Aaron White: Yeah, it’s it’s always a battle. Anybody’s immune system is going to clear some of the curli. It’s just whether it clears at all or not. And in certain individuals, maybe it doesn’t all clear. And then they have problems. But then there’s other people where their immune system does clear it all. I tend to not think of it as they cleared or they don’t. The immune system is always battling and fighting.
Shelley Schlender: The immune system is always battling and fighting. And it’s also always, in a healthy immune system, telling the troops, “It’s okay now. You can go home.” And that’s an important part of the immune system, too. Or, it says to the immune system troops, “It’s okay now. Right now, we want you to put on your medical badge and we want you to go in and start helping repair the tissues.”
Aaron White: Yeah. The ability to activate, but then also just shut itself down and prevent this friendly fire, where they damage the tissues surrounding what they’re actually trying to fight. You’ve got to keep that in check.
Shelley Schlender: Just as a reminder, getting enough sleep, eating food that’s good for your body and good for your digestion, doing things to reduce stress. You might actually be helping your immune system in some huge ways.
Aaron White: Yeah, absolutely. Keeping it in balance.
Shelley Schlender: Let’s go back to these curli proteins that are the furry curly outer shell of a bacteria like a salmonella. There’s another thing that you keep saying, because so far we’ve actually been talking about normal immune response causing friendly fire and all of that. You’ve been using a different word. Aaron White, there at Saskatchewan University. As an expert in immunology, you’ve been using the word auto immunity. That means the body fighting itself on purpose.
Aaron White: The immune system recognizes Curli. But then because of similarities to our own DNA, it starts to cause auto immunity where it starts to actually fight our own DNA. That’s the problem. That’s the auto immunity.
Shelley Schlender: Oh, dear. There’s been a term among scientists and some other folks for decades called 3-way molecular mimicry. (SS COMMENT. April 2000 Science Paper from Loren Cordain about how gut inflammation may be part of inflammatory arthritis.)
Aaron White: Sure. … It is a case of almost mistaken identity where the Curli complex, the DNA shows similar to other things in our body that then our immune system would target.
Shelley Schlender: Something like an undigested protein ends up in the circulation. The body sees it as similar enough to one of the body’s own proteins. Then The specialized warriors’ that it sends out to really take something out like the T cell warriors, they will go, gosh, that’s the bad guy. And this other one over here looks almost like the bad guy. Let’s just say that’s another bad guy.
Aaron White: Yeah. They can’t tell them apart. I’m not an expert in immunology, Dr. Tukel knows more about that. But that’s one of the next things to look at is the mechanisms behind why Curli actually causes auto immunity and what the process is and the involvement of T cells and things like that. But it is a case of almost mistaken identity where the Curli complex, the DNA shows similar to other things in our body that then our immune system would target.
Shelley Schlender 25:16] And that’s auto immunity. You know, there is some evidence that all of our cells work very hard to say what team they’re on. They have little markers that they send up, little flags that say, I’m part of us, I’m part of our human body. And it’s a specialized tag that should be different from what’s on something like a Curli protein.
Aaron White: Yep.
Shelley Schlender: If the immune system’s healthy, it has sharp glasses on. It can really tell the difference between those things, as opposed to having poor vision. Maybe the immune system gets too exhausted. It’s still fighting very hard, but it doesn’t have the ability to discriminate and communicate with other cells enough to tell whether that’s really a good guy or a bad guy. So a tired out immune system that’s been fighting something really hard is more likely to make these kinds of mistakes.
Aaron White: Yeah, it’s, as most things with infection and immune response, there’s many, many factors to it. But certainly that would be one aspect of it, how well they recognize our own molecules as self versus foreign, but also the pathogens that come in. They can turn it upside down, create dis-balance right. And then suddenly know your immune system stats targeting our own tissues.
Shelley Schlender: In auto immunity instead of sending in the medics to say, it’s OK, let’s start repairing things now, let’s cool things off. These exhausted immune system says we’ve got to throw everything we can at this and fight and fight and fight.
Aaron White: Picking up from there. So now imagine a foreign protein that’s clearly foreign that is really, really hard to clear. So it stays there for a long time. That’s the problem. It’s kind of like this constant stimulus to the immune system, these really resistant proteins that have similarities to amyloids, which is another aspect, but also persist for a very long time, can trigger auto immune reactions. And that would be fine, maybe, if that was approaching, that could be cleared right away. But if it’s a protein that can persist in your body for a long, long time, it becomes chronic.
Shelley Schlender: And it makes it easier for the body to start to make mistakes about, It looks so much like these other proteins in me, maybe they’re enemies, too.
Aaron White: Exactly. There’s more chance for errors to occur because it’s this constant stimulation of your immune system. It’s doing its normal natural thing. It’s just maybe that proteins aren’t supposed to be there.
Shelley Schlender: OK. So the paper that you’ve written with that complex title, In Vivo Synthesis of bacterial amyloid curli contributes to joint inflammation during salmonella infection. All of this stems from those observations. And some of this is new, especially the idea that these biofilms of this concretey kind of curli protein could actually be inside the body.
Aaron White: Yeah. That’s. For me, as for somebody who’s been studying the biofilms and the environmental aspects, like how they’re involved in helping salmonella to survive outside of a body, the discovery inside a body is totally revolutionary for me and my research because it opens up this whole area of interactions with the immune system. And so that was the big surprise. I for years thought that these biofilms, you know, we know they’re involved in resistance and persistence. Now, imagining that this might be a normal natural part of a food borne illness, that they form these biofilms before they pass out of the body.
Shelley Schlender: And it’s one of many examples of ways that something that was inside of our digestive tract can end up in our bodies when it’s really not good for it to be inside our bodies, unless we have a healthy digestive tract to keep them out.
Aaron White: Exactly. And to be clear, like we need to do more research on this, but I think salmonella is making these curli and these biofilms for its own end to help it survive, As soon as it passes out of the body. (Ie, getting ready for bright sunshine, dry air, etc on the ground, on water, etc) It’s just unfortunate that these curli proteins are so resistant, and that they are like these amyloid shape. Because they can persist and then perhaps leak out into the tissues. It’s almost like collateral damage. Salmonella doesn’t need to do that. It’s just unfortunate that these proteins just are so difficult to clear and cause these autoimmune responses and potentially even have these interactions with amyloid in our bodies.
Shelley Schlender: It’s not that these bacteria that are looking for food inside of us are saying, “When we leave the body, let’s be sure that we squirt a lot of curli proteins into the tissue to wreak havoc inside this body just because why not?” That’s not how they’re thinking.
Aaron White: Exactly. It’s a consequence probably of just the infection. It’s just unfortunate. And that’s what came to me and to Dr. Tukel as we were writing this paper. Like I said, you couldn’t pick a worse protein from salmonella to be hanging around in your body.
Shelley Schlender: Well, this is a very Canadian attitude. You guys are really live and let live.
Aaron White: Sure. I just think the ability of Salmonella to make the curli doesn’t really appear to help them in the infection. It doesn’t help them, infect better or anything like that. It seems to me, and to other researchers, that the function of the curlis is to help salmonella survive, probably when they’re outside the body (in the air or on the ground). It’s just that our immune system is exposed to these proteins sometimes, and it does maybe bad things to our immune system.

Shelley Schlender Well, thank you. It’s it’s a fascinating area of research. And there’s two ways that my mind wants to go on this. One is I wish I could be little tiny, long enough to go and watch all this happening inside the body. It’s so fascinating that these little tiny things we can’t even see, have these complex lives that they’re living. The other part, though, is on the side. That’s my life and the lives of people I care about. How will medical science and healers use this kind of information to see if they can help people be healthier? Could it be that a naturopathic physician would say, clean up your diet, avoid foods that cause intestinal permeability, and somebody who’s in pharmaceuticals would say, let’s find a drug! There will be a lot of different ways, for better or worse, to try to change the fact that these biofilms probably do form inside our bodies.
Aaron White:Yeah. And, you know, I used the term scary. It’s also helpful to learn these things. Because then as scientists and doctors and pharmaceutical companies, at least we will know more the story of why it’s happening. And then the second you know that, then you can start to work on strategies to stop it from happening. If you know the molecules that are involved, the proteins involved, like these curli, perhaps then we can think of ways to protect ourselves from them in future. And certainly some of my research will be doing that.
Shelley Schlender: How to protect ourselves from the Curli inside our body. These Velcro like proteins that are on the outside of the shell of a bacteria, and find ways that our immune system can be constructive in how it responds as opposed to overreacting and hurting us more.
Aaron White: Exactly. You know, these types of discoveries that maybe open up a new avenue of interactions that we didn’t even know occurred before. You know, you have a target now. Our discovery is uncovering more to this story, helping us determine better ways to treat autoimmunity or inflammatory arthritis, things like that.
Shelley Schlender: Maybe Alzheimer’s, maybe Parkinson’s, maybe lupus, a lot of different things, possibly have some connection to what you’ve figured out.
Aaron White: You know, there’s still lots to be tested and researched. And maybe the scary part is just how similar the structure of these curli is to the human amyloids that are known to be part of Alzheimer’s and Parkinson’s and ALS and things like that. They’re very, very similar. Knowing that these bacterial proteins, these curli, can persist for a long, long time. We haven’t made that connection yet. But it certainly seems logical from a science perspective that it would make sense that these can potentially interact.
Shelley Schlender: Well, it’s probably too early for there to be a consensus about how to deal with this. But I’ll bet you in your Twitter feeds that you’re getting right now, you’re going to be seeing a lot of ideas.
Aaron White: Yeah, for sure. And because I’m not an expert in these human amyloid diseases, I haven’t really delved into it deeply yet. We’ll be collaborating with other scientists who are experts in these other diseases to try and see if there actually is a link and then perhaps how to slow down the process, if it is happening, lots to think about there.
Shelley Schlender: Well, that would be another two days worth of conversation.
Aaron White: Thank you. My pleasure speaking to you. Really good questions. Yeah, it was good.
Shelley Schlender: Thank you for the good explanations and thank you for the research.
Listen here to this extended version of the abridged interview with Ron Rosedale that broadcast on HowonEarthradio April 14, 2020. Transcript is below.
Host/Producer/Engineer: Shelley Schlender
TRANSCRIPT OF EXTENDED INTERVIEW
Ron Rosedale, MD, Talks about COVID 19, the Immune System and Cytokine Storms
DATE: April 14th 2020
Introduction — The Centers for Disease Control reports that people are at greater risk for Covid-19 hospitalization and often deadly cytokine stoems, if they have pre-existing health conditions, such as high blood pressure, diabetes, heart disease. Everyone says that healthy eating might reduce these risks – but does healthy mean the New York Times distractibaking comfort foods of brownies and Nutella shortcake? Does it mean taking dozens of supplements and cutting out fatty junk foods, as Cristina Cuomo recommends for her husband, CNN’s Chris Cuomo? Up next, we talk with Medical Doctor Ron Rosedale about why he believes that eating and sleeping in a way that reduces high levels of the hormone leptin might reduce the chance of severe symptoms of Covid-19, such as cytokine storms.
This is an interview to help you ask questions about the science behind your health choices. This is NOT an interview to take the place of medical advice. Talk with a doctor you trust, if you have questions about your health, and especially if you’re taking medications, and monitor for changes to your need for medications whenever you’re doing a lifestyle change, such as changing your diet.
RON ROSEDALE
Can you hear me?
SHELLEY
I’m using the high tech method of recording this phone call on my handheld zoom recorder as you speak on What’s App from India.
RON ROSEDALE
Yes, I am in India. I’m actually here helping a family known as the Ambani family. Very, very, very prominent. Probably the most prominent, not even probably — they are the most prominent family in India, with their health. And they have they’re mostly located in Mumbai, but ended up getting locked down in a town called Chandigarh. So that’s where I am in a town north of Mumbai called Chandigarh
SHELLEY
We’ve certainly been thinking about India from here in the United States, because there’s so much concern that India’s population density, meaning it’s in great danger from what will happen with Coronavirus. On the other hand, there’s also a thought that perhaps India and Pakistan, because they do tuberculosis vaccines, might have an unusual amount of protection.
RON ROSEDALE
Not just tuberculosis, but Malaria. So, you know, malaria is fairly rampant so many people have taken quinalones, chloroquine, things like that, which is being touted as there is a medication to help treat the Coronavirus. So that’s one way of looking at it.
RON ROSEDALE
However, the most important thing to fight any infection, especially viruses, is going to be a strong immune system. And that’s really the only way epidemics subside. It’s not that the bug goes away, but that people become immune to it. And that’s especially true for viruses.
And the problem here in India is that many people have deficiencies that impair their immune system. So, for instance, whereas in the US, people eat too much protein, which also impairs the immune system, actually, because excess protein is made into sugar. And it raises insulin and it causes what’s called glycation when sugar molecules combine with other proteins and other molecules that impair their function. And antibodies for the immune system are proteins. Protein is very necessary for the immune system. So in the US they eat too much protein, but in India, they eat too little in general, and they don’t have enough protein to actually mount a strong immune system to make antibodies. And so one of the problems with India is a deficiency of protein in general.
And then there’s also some micronutrients that are deficient in general in India, such as B12, which found more in animal products. Many people here are vegetarians. Vitamin D, which people are surprised to hear, even in India. But due to the dark skin, and people who are very modest, so they cover up when they’re out in public, so they’re not exposed to the sun very often, and often it’s really kind of too hot to be outside. And so there’s a gross deficiency in Vitamin D here. And D is very important also for the immune system. And despite having thousands of miles of shoreline, ocean surrounding India. And also because of vegetarianism, they don’t eat very much fish. And so they’re deficient in omega 3 fatty acids, also, which is required to make any new cell, and cholesterol, required to make new cells. So cholesterol is actually a big friend. They’ve shown that a deficiency of cholesterol also impairs the immune system, which also includes taking cholesterol lowering drugs, oddly enough. Not really, oddly enough. But I guess paradoxically, if you want to call it that. So there’s quite a few immune deficiencies in India.
RON ROSEDALE
And then also, from a societal level, people in India really love to congregate. I mean, they’re very, very sociable people. And so they really crowd together. They love being with one another. It’s really nice, but not so much when there’s an epidemic going on. I’m not in general in favor of lockdowns, and we can go into why a little while. But in India, it’s a bit of a different story, because if they didn’t have a lockdown, then the first thing people would do is get together in large groups. And that’s kind of good and bad. A lockdown keeps people indoors, which of course, impairs the vitamin D even more. No sunlight.
RON ROSEDALE
But from an ideal circumstance, what you want, as we were mentioning, to fight any virus is to become immune to it. So rather than hide from it, ultimately we have to be exposed. You don’t become immune to something unless you are exposed. That’s the whole idea of vaccines, for instance, is that it exposes you to the virus or bacteria that then allows your immune system to build up antibodies to it so that you can fight it. Ultimately, that is what has to occur.
The virus itself doesn’t go anywhere. It’s going to continue to be transmitted. Every breath people take at this very moment, they’re breathing in some coronavirus. It’s not the Covid-19 that people are talking about. But the cold virus, influenza viruses. They’re everywhere. And the reason everybody doesn’t get sick and die from breathing these viruses is because they’re built up immunity to it. And what is troublesome about the Covid 19 virus that is affecting people around the world right now is that it’s novel. And so there is no path to immunity to it.
SHELLEY
Our bodies don’t yet know how to fight this particular virus. And we’re right now, with all of the lockdowns, we’re buying some time so that we can see if there’s some way that we can medically intervene either through a vaccine or have better testing so that we at least know who has had this virus and who is at most risk for it. And what the general pattern is for how somebody gets sick. There’s so many unknowns that we’re buying at least a little time with the lockdown is my understanding. Does that fit with what you’re thinking, too?
RON ROSEDALE
Partially. I think that the main benefit of the lockdown is, not that we really don’t know who is exposed or getting tested. I think all of that is really not worthwhile. Everybody’s going to eventually test positive to it. Or the vast majority of people will ultimately test positive to it. And the vast majority of people who test positive will have no symptoms because they have a strong immune system. There are certain predispositions, however, that we do know, and that has to do with diabetes, for instance. We know that the vast majority of people who do have a hard time with this virus have respiratory difficulties, have preexisting conditions. One of the prime ones being diabetes, hypertension, previous respiratory difficulty, cardiovascular disease. And I’ll tell you why in a moment, or at least I’ll tell you why. I think that strokes in a little bit.
But the major reason that a lockdown is beneficial is really not to help people as much, but because this virus is so novel, and many people will get sick because nobody has had the opportunity to build immunity to it, that it overwhelms the medical system. And so, so many people are getting it all at the same time, there will be a fraction of those people who will get quite ill that require hospitalization. And the hospitals and doctors can’t handle the onslaught of such a novel virus. And so, so many people reporting to the hospital being sick, many people need ventilators now, if everybody were to get the infection at the same time, that proportion of people who would get seriously ill wouldn’t be able to get the medical care that they need. And so that’s the benefit of a lockdown is to try and get out the frequency of infection so it doesn’t all happen at the same time. It’s really more for medical care. It’s really more for the hospitals and the doctors than actual people, is really how it turns out.
Trying to hide from this virus is probably futile. As I say, the virus isn’t going anywhere. At some point, people have to go outside and breathe. And we know now, in fact, it should have known before. Surprised me that the World Health Organization expressed surprise that when recently it was found that the virus is in aerosol particles when people breathe, it stays in the air for days. I don’t know why there was such a surprise, because that’s what happens with every virus and not even just viruses, but any tiny particle, like pollen, that’s how people get allergies because they breathe in ragweed pollen, because it’s floating in the air, because they’re tiny particles, and that happens with all tiny particles. So one can expect the Covid virus to be in the air and it’s going to stay in the air. And finally when people go outside, they’re going to breathe. people generally do build an immunity to it. And they’re finding now that the vast majority of people who test positive, if they were to test the general population, and not just sick people. They’ll find the vast majority of people who do test positive have no symptoms at all, that their immune system is up to the task. It fights the virus, and people don’t even know that they’ve been exposed.
SHELLEY
Most people with Covid-19 might feel somewhere between absolutely awful to a little bit under the weather for a little while. But it won’t be as serious as what we’re hearing about so much in the news about people fighting for their lives in the ICU. And if we get an antibody test, if an antibody test becomes available, maybe people would even know if they’ve been exposed and they might be at less risk for both contaminating other people and also for getting as bad a case of COVID-19 sometime in the future. Still unknowns about whether those two possibilities are there, but they’re more likely if someone could get an antibody test.
RON ROSEDALE
Sure. That would be really helpful because then they don’t have to be scared anymore. They can go out dancing in the street.
RON ROSEDALE
Ultimately, the ideal situation is if people were to get something little micro-doses of the virus so that they do build up an immunity because that’s the only way that they’ll ever survive it.
As I say, almost everybody is going to be exposed at some point. And the real competition is really between building the immune system versus the immune system getting overwhelmed by the virus. So if we could be exposed to small doses, that’s a good thing. And actually, as I say, in India, it’s a little bit different because people just tend to congregate together. And so a lockdown in India is probably the only way to slow down the spread of the virus, with so many people, and a medical system that just cannot handle so many people being sick at the same time.
But other than that, it’s probably better to be outdoors, because then the virus will just kind of dissipate into the atmosphere. When people do breathe, they will breathe a small dose of it and they will be able to build up an immune system. And some people will get, like you say, they’ll get a little bit sick. Many people won’t get sick at all. They won’t even know they have it. Some people get a few symptoms. That’s probably, the majority of people get a few symptoms. And then there’s a small percentage of people that will get seriously ill, but only because they have other conditions that impair their immune system or increase inflammation to a great extent.
RON ROSEDALE
I will tell you where, right now, where I think that what the major preexisting condition is and what people can actually do about it. One of the major problems that ends up really killing people and then really, really presenting with the respiratory difficulty, is a mass of inflammation. You know, people have heard of inflammation, where they get swelling due to infection or other things. And injury, inflammation is there to save your life. Yes. The personal immune system.
SHELLEY
People are starting to hear more about the term, “cytokine storm,” and it’s being described as something that does not happen at the beginning of having a Covid 19 infection. A cytokine storm is more when they’ve had the infection for a little while. They’ve had some aches, they’ve had some other symptoms. And then a little later, it’s as though the body goes into another phase of reaction where suddenly the lungs and other body organs are basically fighting themselves. The term cytokine storm is used quite often to describe this very sudden change, where some people are short of breath. Other people, they’re not short of breath, but their oxygen levels go very far down. And whatever symptoms they have at that point, it can mean a very life-threatening situation that has to be dealt with, very quickly.
RON ROSEDALE
Right. And that’s when people need ventilation, when they can’t take in enough oxygen themselves and they need to be hospitalized on ventilators and you’re exactly correct, when you talk about the term cytokine storm. And so here’s what I think ties it all together that I have not read about anywhere. But I think that if I can mention it, maybe people could start researching it. We know that diabetics are very much at risk. People with hypertension are very much at risk. Obesity, obese people are far more at risk. And then there is the cytokine storm that you mentioned.
RON ROSEDALE
Well, there’s a hormone called leptin, and leptin itself is a cytokine.
SHELLEY
What is a cytokine?
RON ROSEDALE
A cytokine is a hormone, essentially, a hormone that acts very locally. They’re very powerful; most of the cytokines are inflammatory. And so, you know, we hear hormones such as thyroid and insulin and estrogen and things like that. But the body has hundreds, maybe even thousands of other lesser known hormones that don’t necessarily circulate 100 percent in the bloodstream, circulate everywhere, but work more locally. (NOTE — “Locally” means that instead of being active throughout the body, a cytokine is released within a certain region of the body, such as in your thumb or in your lungs or heart) And cytokines are sort of like that, although leptin does circulate in general, although it is a cytokine itself. So we know that if you have high levels of leptin, it also causes inflammation. But its major problem is that it elicits the manufacture and the release of other cytokines, one being IL-6. And we know that the major cytokine storm that is occurring with Covid is mediated by IL-6.
SHELLEY
IL-6. That is Interleukin 6. That’s an an inflammatory hormone that the body makes.
RON ROSEDALE
Yes, and it’s very, very inflammatory, and one of the treatments, in fact, one of the main treatments for people with this cytokine storm is to give IL-6 inhibitors, which are given to, for instance, people with bad autoimmune arthritis, for instance, rheumatoid arthritis, which have excess inflammation. So they give IL-6 inhibitors. So the drug already exists, and is being used to treat the cytokine storm because they know that IL-6 plays a huge role in these storms, and I know the strong connection between Leptin and IL-6. When most people have too much leptin, they’re hyper leptinemic. They’re leptin resistant. It’s the major cause of obesity. It’s one of the major causes of diabetes, one of the major causes of hypertension. So all of the predisposing factors that we know exist that put somebody at risk of an adverse outcome with Covid-19 (ie, high blood pressure, diabetes, etc), are tied together by excess leptin. And it mediates hypertension and autonomic system dysfunction. So a lot of these people have a difficult time breathing, not just because air doesn’t get in, but there’s a kind of a central way that people’s almost … wouldn’t say “desire,” because they want to breathe, but they can’t. And not because of obstruction, but because there’s an impairment in their ability to take a breath. And that’s elicited essentially in the brain and hypothalamus. And once again, leptin largely controls the hypothalamus and autonomic dysfunction. And the sympathetic nervous system, vasoconstriction (meaning narrowing of blood vessels), hypertension (meaning high blood pressure). All these things, everything that puts a person at risk for serious disease with Covid has at least partially, if not mostly, to do with leptin. So you want to bring down leptin, and it’s relatively easy.
RON ROSEDALE
You can bring down leptin . . . not totally down to where it should be, because of some of that is mediated by how fat a person is. But what’s not appreciated is that there’s a surge in leptin, a spike in leptin, depending on what a person eats. So if a person eats a high carbohydrate meal, for instance, it causes leptin, that day, to perhaps double, from what it would be if a person hadn’t eaten. So we know that if a person asks, for instance, or if a person follows a low carbohydrate, moderate protein, high diet, that I’ve been recommending for 25 years, that leptin levels will really fall. It can probably go to maybe half of what it was prior to having eaten a poor, high carbohydrate meal, When you lower leptin, I think you can greatly reduce the incidence of inflammation, excess inflammation, cytokine storm, hypertension, all the factors that make surviving this virus far more of a challenge. But this is not recognized. So people go into hospitals, and they get glucose, and everything that occurs, everything they eat inside the hospital, all the IVs they take will raise leptin and make surviving this virus far more of a challenge.
So they take medications to reduce the inflammation, they need to eat also to reduce the inflammation, and to reduce leptin and reduce the IL-6 that’s causing the inflammation in the first place.
SHELLEY
Well, Ron Rosedale, you’ve been giving a lot of information for people to check out about things like leptin, about the role between high blood pressure and high leptin levels, and how the way somebody eats can start to affect the levels of hormones such as leptin. Evidently how someone sleeps also affects their leptin levels. Leptin levels also tend to be higher if someone’s not getting enough sleep.
RON ROSEDALE
Sure.
SHELLEY
SHELLEY
If somebody has suddenly found out that they have symptoms of Covid-19? Is that too late to start sleeping more, and eating in a way that lowers leptin levels? Would it be stressful to the body to shift to these lifestyle changes?
RON ROSEDALE
No. Well, there is a transitional period, and that’s a great question. In other words, whenever the body, kind of shifts gears, then there is somewhat of a stress put on the body, but probably not near as much of a stress as, for instance, a high carbohydrate meal would be caused in raising leptin and raising insulin. And a meal like that raises leptin within hours. And when it raises insulin and raises leptin, we know that it almost immediately increases so-called sympathetic nervous system activity. Basically, the fight or flight stress. And so it’s not a mental stress, but it’s a physical stress.
And you mentioned sleep. One of the major reasons, and probably the major reason why a lack of sleep raises leptin is because of lack of sleep causes an increase in the sympathetic nervous system to keep a person awake. In other words, it causes secretion of adrenalin and noradrenaline from the adrenal glands to allow the person to stay awake when they ought to be sleeping. And that raises the blood sugar. And then the raising of blood sugar, raises insulin and raises leptin, which increases sympathetic nervous system activity, which also then secretes glucose. And you’re into a vicious cycle.
And we know, for instance, and they did this to college students who will pretty much do anything for some meals. They kept college students up for several days straight. And the vast majority of them actually clinically became diabetic. The diabetes was able to be reversed with sleep. But it just shows the power of lack of sleep in causing an increase in blood sugar. That increase in blood sugar is due to an overabundance of adrenal hormones, the stress hormones — hormones of stress, such as adrenalin, cortisol, noradrenaline, things that raise blood sugar. And a lot of that is also then mediated by leptin. And it also raises leptin, again, as I mentioned, a vicious cycle also, with insulin . . . throw that in there also.
SHELLEY
Well, Ron Rosedale with as much as you’re mentioning stress adding to a dangerous situation, we should try to think of a joke to tell right now. But I’m a little short on jokes at the moment!
SHELLEY
Many Americans are on many different kinds of medications for high blood pressure, for high cholesterol, for diabetes, including insulin or insulin lowering medications. When somebody starts to eat and sleep differently, their need for those medications can start to change, so that they can suddenly become overmedicated very quickly. If somebody is not used to eating in a way that lowers leptin levels, would it be best if they work with a medical doctor to help them adjust their medicines?
RON ROSEDALE
I’m really glad you brought that up, because medicines do have to be adjusted, because this is not something that takes days or weeks, but can occur almost immediately, like within hours of changing to a low-carb, high fat, adequate protein diet. So yes, when people bring down their leptin, then they bring down their insulin because of the change in diet again, and again, bringing down insulin and bringing down leptin can occur in one day. Leptin before insulin, actually. It generally does certainly lower fasting blood sugar. So if they’re on diabetic medications, those diabetic medicines have to be lowered. Many diabetics measure their own blood sugar. So that’s easy when your blood sugar start falling. You take less medication. They can probably do that themselves. Great if they can do it under a doctor’s supervision.
Many doctors don’t understand basically the power of diet in reducing insulin and leptin and therefore blood sugar. But great if it can be done under a knowledgeable doctor’s direction.
RON ROSEDALE
The other thing that you mentioned is hypertension, and blood pressure, more often than not, probably at least 75, 80% of the time, will come down fairly rapidly when one drops insulin and leptin, not the least of which is because it reduces the sympathetic nervous system activity, which causes vasoconstriction, constriction of blood vessels and fluid retention, which causes an increase in blood pressure. And so by reducing insulin, which allows the release of retained body fluid, so like when people go on a diet, they know, well, you’re losing a lot of water weight. Yes. You’re urinating away retained fluid, but you’re also then dilating arteries. When this happens, the blood pressure can come down very rapidly and quite significantly. That does also entail a reduction in blood pressure medication.
And so, I would encourage anybody who was on to quite a few medications for blood pressure or for diabetes or anything like that, to home monitor. Get a blood pressure cuff, measure your blood pressure, and as your blood pressure comes down, you can start reducing your blood pressure medication because you can’t wait for a doctor’s appointment, especially at this time when there’s so many lockdowns. So people are going to have to start taking their own responsibility for their health. Many times they’ve been told not to. And so it’s not people’s fault. But everybody wants your doctor to be in charge. And that would be great if they were available, that if they actually knew about such things. But because many of the measurements can be done by people themselves, at home, with blood pressure cuffs, with glucose monitors, it’s relatively easy to measure these things and then recognize that they will not be doing themselves harm. And in fact, doing themselves a lot of help if they can reduce the medications that they’re on, many of which have adverse side effects.
SHELLEY
There does seem to be a strong correlation between people with underlying conditions and having a more serious case of Covid-19 when it does arrive. And yet, I have to say that Ron Rosedale, what you’re describing, even though it’s much more well-known, this topic of a ketogenic diet or a low carb, high fat, adequate protein diet, or even just cutting out a lot of the junk food that people eat, the kind that’s sweet and comfort food . . . ice cream. What you’re saying is not quite consistent with people do in a time of crisis and worry.
RON ROSEDALE
Yeah, and that’s unfortunate. There’s a lot of misinformation out there, especially when it pertains to chronic diseases like heart disease and diabetes and obesity and autoimmune diseases. In fact, I would say that the vast majority of what people have heard about these things is absolutely wrong. And we can see where it’s leading to, you know, heart disease is on the rise. Cancer is on the rise. Lifespan now is going down for the first time in human history. The deeper science that has come out about diet and nutrition over the last 30 some years that I’ve been talking about, this supports the notion that you need to keep insulin and leptin down so that a person becomes more insulin and leptin sensitive. That then allows the burning of fat as opposed to sugar.
RON ROSEDALE
Nutrition itself can boil down to in a very, very simple sentence. Nutrition, health in general. And if I had to integrate literally tens of thousands of research articles that I’ve read, it can boil down into a single sentence. That is that a person’s health and longevity is going to be determined most by the proportion of fat versus sugar that they burn over the lifetime. You can essentially burn two fuels, you can burn fat or you can burn sugar or you can burn products of burning fat, such as ketones. And if you burn fat and ketones as your primary fuel, most of the time, you’re gonna be quite healthy. Your incidence of diabetes and cancer and obesity and hypertension, autoimmune diseases, all of the so-called chronic diseases of aging, and even aging itself, are going to be much reduced. Whereas if you’re burning sugar, most of the time, it will be the opposite. You’re going to be much more disease prone.
Sugar was never meant to be a primary fuel. The reason we have glucose in the blood is not to burn it on a continual basis, but as an emergency fuel because it can be burned without oxygen. So it’s an anaerobic fuel. So if we had to run away from a lion or a tiger and we’re sprinting and we can’t breathe oxygen fast enough to be able to burn fat, then we have sugar because you can burn sugar without oxygen, whereas you need oxygen to burn fat. So it’s a kind of an emergency turbo charged fuel that is there for just that — anaerobic emergencies. But because people constantly eat sugar–by sugar, we’re talking about also foods that turn into sugars, like all of the carbohydrates and starches that people eat, bread, pasta, cereal, potatoes, rice, all of that.
You know, we call them different names and even we even call it complex carbohydrate and think that it’s good for you. But as soon as you chew it and swallow it and initially digest it, it all turns to glucose. It’s your cells that actually do the eating. So we think of ourselves as putting food in our mouth, chewing it, and we’re eating. But we’re not, we’re just processing the food, ultimately making little molecular pieces out of it so that we can feed ourselves. So whether it starts out as as rice, potato, cereal, and then we put it in our mouth and we chop it up into smaller pieces and swallow it and then we we basically chemically “cook it,” and we make it into even smaller little molecular pieces to feed our cells, who actually do the eating, what they’re going to see is glucose. And so that’s what we’re feeding them. We’re feeding them glucose.
It doesn’t matter what our perception is, when we put it in our mouth. While it circulates, and it’s glucose, it also raises insulin and raises leptin, and our cells then become bombarded with insulin and leptin, day in and day, out almost 24 hours a day. Ultimately, the signal, the really critical, life-giving signals of insulin and leptin become corrupted because they’re overused. It’s like being in a smelly room too long. Pretty soon you can’t smell it. And so there’s you know, there’s reasons for this. And so people become insulin and leptin resistant. And that produces even more insulin and leptin because the body wants to get those life-giving messages heard. And so it produces more insulin and more leptin. But the problem there is that there’s an orchestration, whereas, for instance, with insulin, we want your liver to essentially get a higher signal than your fat. But as you become insulin resistant, your liver becomes resistant first, and then it can’t hear insulin’s message. So it makes too much sugar, so diabetics wake up in the morning, haven’t even eaten, and their blood sugar goes up rather than down. And that’s because the liver has made too much blood sugar, because it can’t hear insulin, because it’s insulin resistant, and the orchestration of insulin becomes corrupted. And so the fine orchestration of signals in the body becomes impaired. That’s what causes disease.
SHELLEY
A new novel virus such as coronavirus-19. adds another way to make a lot of noise in the whole system.
RON ROSEDALE
Absolutely
RON ROSEDALE
Something like coronavirus will bring out deficiencies in our health. You know, it becomes very apparent when a person’s immune system is impaired, and the person’s immune system will be impaired when they are leptin resistant and when they have high levels of leptin, which occurs because of that resistance. Leptin itself, although better known to be a hormone that regulates fat metabolism and fat storage, we know that leptin is elevated in almost all obese people, what is not appreciated is how important it is for the immune system.
The white blood cells, which are critical to our immune system, have leptin receptors, in other words, leptin signals white blood cells very extensively. And so when a person’s (cells) can’t listen to leptin properly, their immune system is automatically impaired. So they can’t fight the infection as well. And then in addition to that, what we talked about is the high levels of leptin predispose to this so-called cytokine storm because it makes too much IL-6 to begin with. And leptin itself is a cytokine and is itself inflammatory. So when it’s high, they body’s already too inflamed. And then the predisposition to manufacture and secrete IL-6, which causes even more inflammation, which also then raises blood sugar . . . so you get all these vicious cycles.
So, yes, you want to try and improve your health as much as you can. And your immune system is certainly going to be a huge part of that. And so improve your health in general. One of the main ways is by burning fat as your primary fuel, as opposed to sugars. And the only way that you can do that is by having leptin and insulin being signaled properly. People have to look at eating as, it has nothing to do with calories. You want to eat to regulate the hormones, such as insulin and leptin, that then tell your cells what to eat, i.e., sugar or fat. You don’t just, burn what you eat. You have to go through a whole complex symphony of metabolic orchestration that then tells your cells what they should be eating. And they’re the ones that actually do the eating. And that is what your health depends on. So, again, you eat to regulate insulin and leptin that then tells your cells, whether they should be burning fat or burning sugar, which then has a huge amount to do with inflammation in general and health in general and whether you’re going to be able to fight off his Covid virus or not.
SHELLEY
And so you want your body to be able to fight this new virus and figure out the way to fight it. But you also want your body to know when to not OVERfight, not to fight so much that it causes the cytokine storm.
RON ROSEDALE
You don’t want a bunch of collateral damage. You don’t want your immune system to just start flailing around like a berserker with a sword and killing all the people around. You want to specifically kill the Covid virus, not your own cells. And when the immune system is dis-regulated, what you’re getting is a whole bunch of collateral damage. Your own cells die. You’re killing your own cells as opposed to the virus. Obviously, that will not lead to a very good outcome. So inflammation has to be controlled. And we certainly need inflammation to be able to fight anything, any kind of stress. But certainly you need inflammation to fight viruses. And fight bacteria. But again, it has to be controlled properly and to control it properly. Insulin and leptin have to be controlled properly. And to control insulin and leptin properly, you have to eat properly.
SHELLEY
Leptin levels tend to be higher in somebody who is overweight or obese. Does it take losing 20 pounds to create this protection. What makes this protection more likely is to get enough sleep and to eat in a way that doesn’t push the body into lots of leptin and lots of insulin.
RON ROSEDALE
Yeah. And again, an excellent point, and this is something that is misunderstood, especially by most doctors and even the people who know about leptin. Many people feel that leptin levels are determined by how much fat a person has. And that’s partially true. The more fat you have–most leptin, not all — most leptin is produced by fat itself. And so it’s thought that the more that you have, the higher your leptin and the only way you bring down leptin is by losing weight, and that you can only bring down leptin by losing weight. And of course, that is a many months long process. That’s not true. Your leptin levels are determined by two factors, not just one, not just by how much fat you have. How much fat you have kind of sets kind of a baseline level. So if you are fat, you will have a higher baseline level. But that baseline level can dramatically rise, depending on what a person eats for breakfast or lunch or dinner. And that can be controlled, almost immediately. Change what you have for breakfast, lunch or dinner and you can cut your leptin levels almost half in one day. And that’s been shown for many years. But it seems still to be unknown to people that you can greatly bring down your leptin. And when you bring down your leptin by preventing the big surges, the big spikes in leptin caused by what a person eats, then you increase the sensitivity, you reduce leptin resistance, and when you reduce leptin resistance, you’re allowed to burn fat. And then, over a longer period of time, you start burning your fat, and then leptin goes down even further. That takes a while, but it doesn’t take a while to bring leptin down dramatically. Very quickly, just by changing what you eat, when you mentioned that leptin tends to be higher in obese people, I would actually go a little bit more emphatically with that, and say that leptin, almost always is higher, in overweight and obese people. It’s very rare for an obese person not to have higher leptin. There are very, very rare genetic mutations that a person might have. But that would be, probably less than one in a thousand. So the vast majority of people who are overweight and obese have high levels of leptin. And they can bring those down, as I say, within one day, if they eat properly. They won’t bring it down all the way. You know, they won’t bring it down as far as we like. That would entail some fat loss. But certainly by bringing down the spikes in leptin, you can improve dramatically, very quickly. And then it also then allows you to burn fat, so that over the long haul, you can bring it down even further as you lose your excess fat, especially your visceral fat, belly fat. It’s the belly fat, we know, that produces a lot of these inflammatory chemicals, such as IL-6, that causes over inflammation and predisposes to diseases such as diabetes and auto immune diseases. And the cytokine storm that you were referring to earlier.
SHELLEY
If somebody has a higher weight than they think that they should have, or if they’ve been told that their obesity is a is a danger to them, that simply by starting to eat differently, they’re significantly changing the inflammatory response in their body to one that is not going to be as much of a roller coaster, that will probably fight the virus better, but also not create a cytokine storm. There’s three things that I think we could give people as take away points from what you’ve said.
RON ROSEDALE
It’s always best under an educated doctor’s supervision. Right. Somebody that actually understands the changes that occur when a person changes to a diet like we’ve been recommending for decades. So that would be ideal, but I wouldn’t necessary dependance really. As you say, it depends on the doctor. Totally depends on the doctor. There are some doctors that are very knowledgeable. It would be great to listen to their advice. And there’s other doctors who know very little about this and whose advice actually might be more harmful than not. So it’s really hard to say. But one thing I would urge people is to take their health in their own hands. Read a little bit about what leptin does. Read a little bit about the power of a low carbohydrate, high fat diet, which now being called a ketogenic diet, which I don’t agree with the name. It’s not the ketones that are so beneficial, but the actual burning of fat. And don’t be afraid really to adjust your own medications. If your doctor is unable to do so, if your doctor does not really know about the physiology for instance, of insulin and leptin and what it will do to the blood sugars. If your blood sugars fall. You must reduce your blood sugar medication. Reduce your diabetic medication. It’s really quite simple. Start off slow. If blood sugar stays high. Reduce it a bit more. Same with blood pressure. If your blood pressure is going down, reduce your blood pressure medication. Don’t be afraid to do it. Great If you can talk to your doctor, and he can, maybe if you’re on multiple medication, he could tell you which medication might be best to reduce to begin with. But if you, for instance, can’t get ahold of your doctor because they’re so busy because of the viral infections that are going around, then take your health in your own hands. It’s not really that hard to do.
SHELLEY
If they do feel like they need a doctor’s advice, if they could start calling today to interview different doctors and find one who they could shift to, who could walk them through this. There’s an increasing number of agencies and places that offer ways to coach people on how to eat in the way that you’re describing.
RON ROSEDALE
Absolutely. There’s even like online apps that can help people in this sort of thing. So there’s certainly help out there. And a person just has to be diligent and look around. As you say, interview, interview doctors, look at different websites. But I think that certainly the situation right now calls for self education, you know, educate oneself about what they can do on their own to take their own health in their own hands. You’ll know your health better than anybody. You’ll know what your blood sugars arel you’ll know what your blood pressure is. You’ll know what it is this hour, because you might not be able to call your doctor this hour. So I would certainly recommend a person going and purchasing a blood pressure cuff and a blood glucose monitor. Those are the two indexes that can change quite dramatically when they change their diet and need adjusting as far as medication for sure.
SHELLEY
Well, good luck with what you are doing yourself. Have you had this virus yet that you know of?
RON ROSEDALE
You mean have I personally?
SHELLEY
Yes, have you had Covid-19 as far as you know?
RON ROSEDALE
No. I’m actually locked down in a beautiful facility, actually, so I can’t really complain. I’m taken very good care of it. Right now, there’s virtually no chance that I could be exposed. So I have not had it. I actually would like it. That might sound funny to say. But I would like a low dose. I would like to actually be exposed to a little bit, because I know eventually I’m going to have to be. And I would just as soon be exposed a little bit so that my immune system would start building up tolerance and building up immunity, building up antibodies and building up white cells to the virus, so that when I do get a bigger exposure, you know, it’s not going to affect me so much. So as I say right now, where I am and I think in India, I don’t necessarily disagree with the advice for a lock down only because in India there are so many people, and the medical system can be so easily overwhelmed. And because the society here is so social. I mean, people just love to congregate, that I think the prime minister didn’t have much choice but to kind of insist on a lockdown to keep people from spreading it so fast that would overwhelm the medical system. But I think in most countries, I kind of agree with the approach, that Sweden has taken, which is just actually go about your business. But pay attention, keep your distance. Wash your hands. Don’t cough on people. If you have it, stay on there. They seem to be doing just fine. I think that probably for most countries, including the U.S., I think or at least most places in the US, would do probably better, with that approach, than trying a more complete lockdown. In other words, don’t be afraid of getting it. You just don’t want to get a high dose of it. You know, you don’t want people to sneeze on you or you don’t want to sneeze on other people. Or cough on other people.
SHELLEY
And, you know, there is new evidence that indicates that people get the highest, most virulent dose of it. When people are early on in the infection and may not even have symptoms, which is quite a different thing about this virus, that it’s at its most potent when it’s early on, that’s when it’s most likely to be shedding and spreading. Probably an exception is if somebody is in the hospital and having to be intubated for a ventilator. Somebody who’s doing that from a health care perspective is very much at risk because they’re just so close to somebody. But in just general hanging out with people, it’s when people don’t have symptoms, and it’s early on that they’re most likely to spread this virus, which would mean that the more that people get lots of rest and eat, not for comfort, but for health, it might be a smart idea to do those things.
RON ROSEDALE
I think that’s exactly correct. Once again, that the major superpower, I guess, of this virus is that it’s new. So people have not developed an immunity to it. And therefore, early on, like you say, it’s going to be much worse because people have not yet developed an immunity to it. So the more a person has the virus, the more, if they have a good strong immune system that build up antibodies against it that will be able to engulf it and kill it. So then it becomes less virulent, as time goes on in a particular person and then over the weeks and months between people, as people start developing an immunity to it. But early on, when that immunity is lacking, certainly the virus becomes the most contagious and the most powerful because the immune system is not fighting it then.
SHELLEY
Yes. And so here we are in this situation where it would have been so fun to talk with you additionally about what just what is going on. How does the immune system fight things? What is the mechanism of what causes high blood pressure? We could have had a fun conversation about those things, too, but right now what’s on people’s minds is how do they do what they can to protect themselves? How do they do what they can to share information with a loved one that they care about that they’d like to have around in another year? These are real questions that people are facing.
RON ROSEDALE
Yes, absolutely. Well, you know, for me, eating properly is paramount in any disease. But certainly the chronic diseases of which an impaired immune system is one which then can manifest and is brought out by this virus. You want to eat properly. In addition to eating properly. There are certain micronutrients a person can make sure that they have enough of such as vitamin D. That’s why staying indoors sometimes might be counterproductive because certainly the best way to get vitamin D is to get sunlight. So I would not be afraid of going outside.
And also, as you go outside and you’re breathing, your aerosol particles will dissipate into the atmosphere. So they’ll become less concentrated, whereas indoors they’ll become more concentrated. So being indoors might not actually be the best thing. Outdoors, it’s fine as long as you don’t congregate with people so that, you know, they’re not directly getting a huge dose of coronavirus. Let it dissipate off into the atmosphere. So keep your distance a little bit or. You can take certainly take very easily, Vitamin D soft gels.
SHELLEY
You still think that outdoors is best. And for people in Colorado where this will broadcast, what a beautiful place to be outside and people are learning to keep their distance from each other during this virus crisis.
RON ROSEDALE
Exactly. I think being outdoors is great. I would encourage it. that the fact that there’s more awareness than it can be an aerosol is why now the Centers for Disease Control is recommending face masks.
Yeah, well, I it actually surprised me more than anything when the World Health Organization a week ago or so was surprised that Cauvin can be in the air for days. I was surprised that they were surprised because that’s pretty well known on almost all viruses. For instance, influenza is known to be in the air for days. I don’t know why this virus would be any different, but anyway. I would certainly encourage sunlight, encourage open air. Make sure you do get enough vitamin C. I don’t necessarily believe in going overboard with it. There are downsides to taking too much, but something like 500 milligrams or so twice a day or high. I particularly like the form of vitamin C.
Podcast: Play in new window | Download (Duration: 40:46 — 37.3MB)
Subscribe: RSS
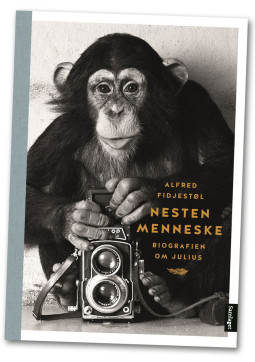 Almost Human – The Story of Julius, the Chimpanzee Caught Between Two Worlds (Extended Version) by Alfred Fidjestøl. This is the full version of the interview.
Almost Human – The Story of Julius, the Chimpanzee Caught Between Two Worlds (Extended Version) by Alfred Fidjestøl. This is the full version of the interview.
Podcast: Play in new window | Download (Duration: 27:43 — 25.4MB)
Subscribe: RSS

Low Carb Diets and Longevity – Ron Rosedale, MD – Extended Version Dr. Ron Rosedale, MD, gives a “second opinion” about a widely publicized report in the prominent medical journal The Lancet. The Lancet report contends that low carb diets (40% carbs or less) shorten lifespan, and moderate carb diets (roughly 55% carbs) promote longer lifespans. The study is being hailed as proof for why people should “eat carbs in moderation.” But what if the Lancet study didn’t go low enough on carbs to reveal potential benefits of a VERY low carb diet? Dr. Rosedale advocates a very low carb, adequate protein, high fat diet, meaning roughly 15% of calories from carbohydrates, 15% from protein and 70% from fat. – Producer – Shelley Schlender
TRANSCRIPT
Shelley – Ron Rosedale what is it about your background that means that you can be somebody who speaks to the idea of low carb diet and longevity.
Ron Rosedale – For the vast majority of my professional career, that’s what I’ve been studying. And I believe at least in the U.S. I was the first person to actually recommend and utilize a high fat low carbohydrate diet to treat a multitude of the chronic diseases of aging and have been studying the biology of aging for my entire adult life. So what my interest has been has been in the dietary connection to the hormones and pathways that are known to influence, if not regulate, the biology of aging teeth. That’s really what one has to look at if one is going to evaluate the health of any particular dietary or interventional regime–how does it affect aging and mortality.
Shelley – Here is a study that came out recently from the Lancet the journal Lancet about just that topic. That longevity study seems to show that people who eat a low carbohydrate diet die sooner than people who eat moderate carbohydrate diet.
Ron Rosedale – Well first of all ,had they stuck to the title of the study, where it’s different amounts of carbohydrates versus mortality, if they had if they had not used, later in the study, the word “low carbohydrate” it would have been a better study because the problem is that they didn’t study a low carbohydrate diet. So here they are then making conclusions about a low carbohydrate diet, which is you know, picked up everywhere about low carbohydrate diet. And they didn’t study a low carbohydrate diet. Not at all.
Shelley Schlender – In the Lancet study the amount of low carbohydrate that they were looking at was 40 percent or less. You say that that’s not a low carbohydrate diet?
Ron Rosedale – No. They lumped it all into — I think the the lowest quartile was 37 percent. That’s not low carbohydrate at all. In fact that’s probably the worst diet, and that’s what their studies showed. I think the worst diet is one where you mix, kind of, an equal amount of carbohydrate and fat. And the reason it’s the worst is because carbohydrates turn to sugar, then the sugar goes up, and it raises insulin and when you raise insulin, your body can’t burn fat. If you summarize all of nutritional science you can do it in a single sentence. And that is that, one’s health and lifespan is going to be more determined by the proportion of fat versus sugar that a person burns in a lifetime than anything else. The key is to burn fat. And if you eat 40 percent, or 37 percent carbohydrates, you will not be able to burn fat. That’s why people are getting so fat—people get fat not because they eat fat but because they can’t burn it.
Shelley – What stops them from burning the fat?
Ron Rosedale – When you eat a bunch of carbohydrates, and a bunch to me it would be 37 percent. That’s a lot of carbohydrate. Really. This will raise specific nutritional pathways and hormones. People have heard about insulin and I first started talking about the connection with insulin and disease many many decades ago and now it’s becoming more commonplace. Still, we knew even a quarter of a century ago that when you raise insulin it prevents the burning of fat. And so when you eat carbohydrates, the carbs turn into glucose, you raise insulin and you can burn fat. It’s as simple as that. But you also you also raise leptin and you also raise another even more critical pathway called the target of rapamycin that hardly anybody knows about right now. All of these conspired to make a person store fat and not burn it. And that’s always a awful and that’s where you can run into higher mortality and that’s what this study found.
So what this study really showed was that a medium carbohydrate diet, so a diet that consists of high fat and high carbohydrate or you might say medium-fat, medium-carbohydrate, however you want to say it– there was no low involved anywhere that will be unhealthy. And they found also who they should use for them to eat a very high carbohydrate diet. That’s also very bad. So they found two bad groups. One was a medium carbohydrate kind of medium fat diet that’s bad lead to higher mortality and if you eat a very high carbohydrate diet that’s also bad. It’s basically what they found there was no there was no low anywhere, other than the very high carbohydrate diet was what you might call a very low fat diet. And that they found to be very detrimental and lead to higher mortality.
Shelley – What would you consider to be a true low carb diet. If 30 percent or excuse me if 37 percent is not a low carb diet what is what is?
Ron Rosedale: You’d have to get down to about 15 percent. Up considerably lower than what they were testing at. George Cahill at Harvard showed this — that if you don’t get down that low you’re not going to efficiently burn fat. You’re really not going to burn fat as your primary fuel unless you get down that far. And the reason for that is the reason we stated about the effects on hormones. So you really have to get down there. A major problem with this study is that, first of all I mean there are a lot of things, there’s so many problems with it. Not the least of which is what we talked about there when there was no low carbohydrate diet group to begin with.
And the reason for that is, what they studied, it was an epidemiologic study. It was a population study. Epidemiologic studies are difficult to begin with because they have so many variables that you have to account for if you can. The problem is you can never account for all the variables because you don’t know all variables nor do you typically get data on all the variables. In this particular study it was a questionnaire. And so number one is an epidemiologic study. Number two they used questionnaires and many studies have shown that when you ask people what they’ve eaten, especially when they have to reflect on it, if you ask the question, “What did you eat last week; what did you eat yesterday?” They’re notoriously wrong. And you can speculate as to why they’re wrong. Many people feel guilty for instance if they ate two milkshakes yesterday and french fries, they’re not going to report that–they might report one milkshake. They didn’t report that they ate too much. There’s kind of a guilt and especially when it pertains to higher fat. You know that the fat has been so vilified that people are just reluctant to admit that. So anyway whatever the reason we know that food questionnaires are fraught with inaccuracies. So that’s another problem with this study. It began in the 1980s and in the 1980s there was there was no such thing as low carb–that it wasn’t even a phrase. So virtually nobody was eating low carb because everybody was told that that you should eat high carbs. And that’s a major major problem then with an epidemiologic study. Also, we mentioned that there’s a lot of confounding variables, and in this study there were at least at least one major one. Actually are two major ones. One you can’t blame them too much for, because in the days when this data was collected, they just didn’t know anything about TOR (the target of rapamycin), but they did know about Ferritin.
Ferritin–too much iron is very bad for a person. If it accumulates we know that iron rusts, for instance and it actually literally rests inside your body too and it can kind of rust the lining of your arteries and burn the lining of your arteries. It stores in tissues such as the pancreas and we know that high ferritin is very associated with diabetes. Ferritin is a reflection of how much iron a person eats. I knew when I was seeing diabetics every now and then you’d find a diabetic with a very high Ferritin levels and you could literally reverse that person’s diabetes if they did nothing else, just by lowering their ferritin. And so ferritin is also very highly correlated with mortality.
Shelley – What is there diet that tends to lead to higher iron levels, high ferritin levels.
Ron Rosedale – Great question. The major factor, really about the only food that can really shoot up ferritin levels and iron levels, and this can be a an additional factor that causes a greater rate of death i.e. mortality, is red meat. And so people who eat a high red meat diet have to really measure their ferritin, but it’s just rarely done. There’s no money in it for anybody. There’s no drug that really lowers your ferritin, and so it’s not paid attention to. But it’s a really simple variable that can be accounted for, certainly in a study like this — it’s there but only indirectly — the study conclusions did point out that people who got their protein from plant-based sources tended to live significantly longer than people who got their protein from animal sources. A lot of animal based protein comes from red meat which contains high ferritin. And that’s really the point that we’re making–the researchers came to the conclusion that animal-based protein is more hazardous, because in their statistics they did not account for ferritin. That’s even though the association with ferritin and mortality is well known. In other words had they corrected for ferritin levels I think they would have it would have negated the difference in results they had with mortality in a plant based versus animal based diet, because there’s such a high correlation of mortality and ferritin. They came to the conclusion that animal protein was bad as opposed to plant protein, but that was a false conclusion I believe. Ferritin, they didn’t account for that. Had they accounted for that I think it would have eliminated the vast majority of their (negative) results (regarding animal versus plant protein). It would not have been the protein source that led to higher mortality–it would have been the iron. The animal protein consumed was mostly red meat which is lamb, beef even chicken to some extent has red from blood. And that raises ferritin, but they didn’t measure ferritin, and they didn’t compensate for that ferritin when they came to their mortality conclusion. ((NOTE – For someone who has high ferritin levels, Ron Rosedale recommends giving blood to reduce high iron levels)
The other major confounding variable that was not accounted for and this is probably because they didn’t know anything about it. And that’s again a problem with epidemiologic studies that you can’t account for things you don’t even know about. It had to do with a pathway called the mammalian or sometimes now it’s called mechanistic, and you should even forget about the I think. It should be called the target of rapamycin. That’s a newer pathway that is now extensively being studied. It’s a pathway that now has been attributed to the longevity and health benefits of calorie restriction diet, for instance. So it’s an extremely important pathway. It’s a very ancient pathway that regulates almost all life metabolism. The pathway is influenced by all sorts of different nutritional inputs, such as the amount of energy, the amount of ATP which is kind of an energy battery, insulin, leptin but it’s also influenced by nutrients. The most powerful stimulant of Tor is protein. The most powerful stimulants within protein are the branch chain amino acids and particularly something called leucine, which is a particular amino acid that is found much higher in animal protein. Animal protein has long been considered a much higher so-called quality protein — that’s how it’s described in scientific journals. In contrast, plant proteins are deficient in many essential amino acids ((Vegetarians get complete proteins by eating complimenting foods together)). But the relevance here is that plant proteins don’t elevate the target of rapamycin near as much as animal proteins.
Shelley – Is it good or bad to have high TOR?
Ron Rosedale — Well it’s probably good early in life. This would get us into probably a longer talk than we have time for as far as the biology of aging. But prior to reproductive years it’s good to have higher TOR because you need it you need to grow. You need to grow muscles and you need it just to grow up, so that you can become an adult. But after reproduction — basically after middle age, then an elevated TOR starts causing lots of problems and we know elevated TOR can increase risk of cancer and an increased risk of death from other causes as well, which is why lowering the Target of Rapamycin is more known today. There is even a drug that lowers it. And we know that that is the first drug that actually has been shown to lower TOR also very convincingly reduces the rate of aging in laboratory animals. That’s pretty cool. So in other words TOR really is a powerful pathway, and it high TOR raises its ugly head after middle age. If you raise TOR after middle age, it increases the risk of cancer, and it increases risk of mortality.
Shelley – What I hear you saying is that if someone is eating a lot of protein after middle age, they increase the likelihood that their TOR levels will be high. And if somebody wants longevity they might want to have moderate but not too much protein–ie, less than most Americans eat, in order to give them a better chance at longevity.
Ron Rosedale – That’s exactly correct. But in this study what is particularly relevant is you can eat more plant protein without raising TOR, compared to eating the same number of ounces of animal protein. That’s because plant protein is “lower quality” it’s less usable, and so you can eat more of it because eating more plant protein is like eating less animal protein.
Shelley – The Lancet study does seem to indicate that people who ate plant based proteins were more likely to live longer than people who ate animal based proteins.
Ron Rosedale – That’s correct. But the confounding variable that they did not account for was the quality of the protein, in terms of them measuring the “amount” of usable protein in plant versus animal protein. To figure that out, they could have just measured the amount of leucine–it’s actually quite easy to measure in a food-based analysis. And rather than saying that animal protein leads to higher mortality they could have just said that eating too many much branch chain amino acids, for instance, will lead to higher mortality, and that’s probably true. In other words, it’s not the fact that it is an animal or a plant. It is the fact that you have more usable protein in the animal protein.
Shelley – And people in the United States tend to eat an excess amount of protein compared to what their body actually needs?
Ron Rosedale – Exactly. And that will lead to higher mortality. In the same vein, the other reason that, calorie for calorie, a plant based diet can show greater benefits than an animal based diet is because a plant based diet is much higher in cellulose. Cellulose is the stringy part of, let’s say celery. Cellulose is fiber. It’s not digested. So you hear the adage you are what you eat. But that’s not really true. What is much more true is that you are what you don’t excrete, and when you eat a bunch of plants, basically some “calories” are actually fiber, and they go right through you. You basically poop most of it out and so you don’t really eat it; you don’t absorb it. And so it’s a way to eat less without it being counted as eating less.
I don’t care whether a person eats plant or animal protein. It doesn’t make any difference really–what is important is the amount of absorbable protein, and the amount of absorbable carbohydrate. And the same can be said for fat. And so that’s what needs we can in other words what are you really eating what are you eating that’s actually getting absorbed and doing something. And yet if it just goes in and out of you it’s it shouldn’t really be counted. And so if you eliminate that portion what you’re really seeing is that if two groups eat the same so-called calories in one group is eating a bunch of cellulose from plants they’re actually eating them they’re actually eating much less. And so that wasn’t accounted.
Ron Rosedale – Also the types of fat weren’t accounted for. And that’s easy to measure. We know the benefit for instance of fish oil and how much omega 3 someone eats, whether from plant or animal sources. How much mono unsaturated versus polyunsaturated fat for instance. Walter Willett ((author of this study)) he’s done a lot of great papers but this I think was not his greatest hour.
Shelley – Would you like it if the researchers would make available the entire database of what they collected over 25 years in these informational interviews, to see what else could be teased out of the study from people looking through different lenses?
Ron Rosedale – My guess is they would have they would have then come to no conclusions. I think it would have shown nothing because of the the other factors. For instance, even if they did have a very low carbohydrate branch in this study, there would probably be too few who ate that way for statistical analysis because, really nobody was eating a very high fat, very low carb, adequate protein diet in the 1980s. And that’s the other major problem in that you know we haven’t even talked about the major problem in this study. Now Einstein once said that you want to keep things as simple as possible but not too simple and you don’t want to keep things too simple because it will make it wrong. And what they did in this study, is they kept things too simple. You can’t just measure the amount of carbohydrate and compare it to everything else. When I first started talking about high fat – low carbohydrate diets in the late 80s and early 90s, nobody was talking about it then. But I knew even back then and there were maybe four or five other people in the world that were talking writing about low carbohydrate and they were all high protein. But at the time people didn’t really pay that much attention because they were just thinking about low carbohydrate. But since we now know, and I’m very happy because I’ve been pushing a high fat instead of a high protein diet for the last quarter century, there’s a huge difference between a low carbohydrate high fat diet and a low carbohydrate high protein diet.
And the vast majority of people who were undertaking a low carbohydrate diet since they started since we started talking about it in the late 80s and beyond, they gravitated to a high protein diet because fat had been so vilified. It’s only been very recently that the the falsity of the detriment of high fat is coming to light. They’re not even talking about low carbohydrate diet anymore. They’re talking about ketogenic diets and that’s also a name I’m not really fond of ((because consuming excess protein can increase ketone production as well)), but they talk about it because in general, ketones are chemicals that are produced when you burn fat. It’s not the it’s not the fact that you’re eating low carb it’s the fact that you’re allowing the burning of fat and that allowing the burning of fat is what we talked about earlier. By regulating hormones that tell you whether you can burn fat, it regulates insulin and leptin and Tor, so you eat to regulate the hormones that tell you whether you can burn fat or not.
And so you can’t just talk about low carbohydrate and compare it to everything else which is what this study did. And that’s really the major problem with it. So not only did they not have a low carbohydrate diet, but they then lumped low carbohydrate with anything else. They didn’t tease out: Was it a low carbohydrate high fat? Was it a low carbohydrate high protein in their mortality statistics? They didn’t tease it out.
Shelley – Are you concerned that this kind of study and the way that it’s been reported, ie publicity asserting that you live longer you eat over half your calories is carbohydrates–this may scare a lot of people into avoiding trying a very low carb diet?
Ron Rosedale – Yes I am very concerned. I think that papers such as this are extremely dangerous because diet is so important to a person’s health. I mean everybody’s heard that you know. Yeah what they eat is important. People don’t understand how important it is. By influencing diet in laboratory animals you affect the rate that they age. That’s huge. You affect the most important pathways in the body that regulate cardiovascular disease and cancer such as the TOR pathway. What you eat is extremely important. And so people authors such as this have to show greater responsibility.
Shelley – If you were to start this kind of study today to get the kind of information you think would be of use to people, what would you do?
Ron Rosedale – Well the problem is it’s very difficult to do human mortality studies because you have to wait at least a generation. You know it would be a study that would take 50 years and most people don’t want to wait that long. Certainly most researchers don’t, because the results of the research wouldn’t come in until after most of them had died. But you can glean at least something from animal studies. The basic pathways that regulate metabolism have been around almost since animals have evolved and the reason for that is those pathways are so important that they they weren’t mutated away. Any type of major mutation to these major pathways would have led to death, so that species wouldn’t be around today. So the major pathways, the major metabolic hormones Tor and insulin and leptin, they’ve been around for a very long time.
Shelley – What do you recommend for health — 15% carbs, 15% protein, 70% fat?
Ron Rosedale – (YES — HOWEVER . . . ) if you are going to go on a low carbohydrate diet you really have to go on a low carbohydrate diet. You can’t do it. Well I don’t know if I can say this on air but you can’t do it half assed You’ve got to do it. You’ve got to go on a low very low carbohydrate diet and substitute good fats into the type of fat make a big difference. And so it has to be done properly. You can’t just do it haphazardly and you can’t do it half assed. You just have to do it and then you’ll see huge benefits. Best thing you can do.